You are viewing 1 of your 1 free articles
Hip weakness and shin splints: a biomechanical approach

Medial tibial stress syndrome (MTSS - commonly known as shin splints) is not medically serious, yet can suddenly side-line an otherwise healthy athlete. Roughly five percent of all athletic injuries are diagnosed as MTSS(1).
The incidence increases in specific populations, accounting for 13-20% of injuries in runners and up to 35% in military recruits(1,2). MTSS is defined as pain along the posterior-medial border of the lower half of the tibia, which is present during exercise and (usually) diminishes during rest. Athletes identify the lower front half of the leg or shin as the location of discomfort. Palpation along the medial tibia usually reproduces the pain.
Causes of MTSS
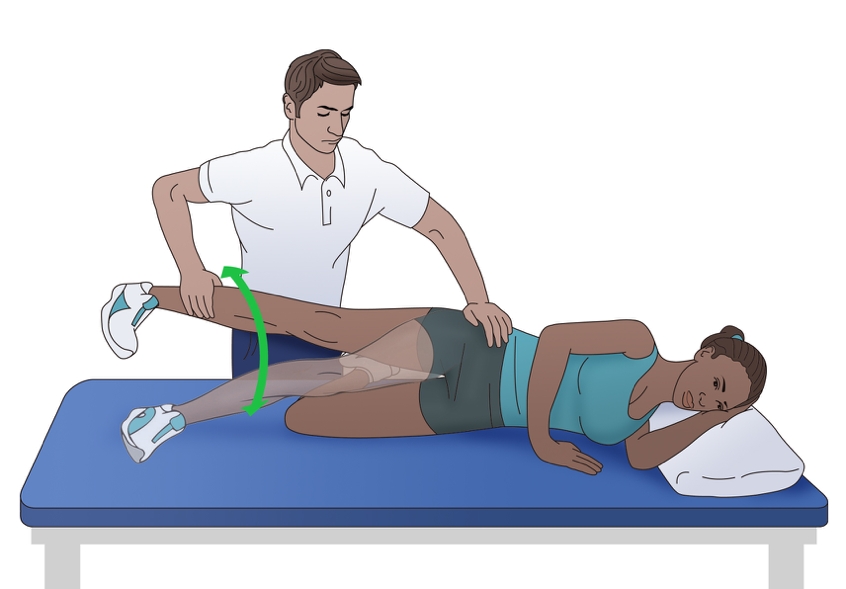
There are two main hypothesised causes for MTSS. The first is that contracting leg muscles place a repeated strain upon the medial portion of the tibia, inducing periostitis - inflammation of the periosteal outer layer of bone. While the pain of a shin splint is felt along the anterior leg, the muscles that arise from this area are the posterior calf muscles (see figure 1). The tibialis posterior, flexor digitorum longus, and the soleus all arise from the posterior-medial aspect of the proximalhalf of the tibia. Therefore, the traction force from these muscles on the tibia is unlikely to be the cause of the pain typically felt on the distal portion of the leg.Figure 1: Anatomy of the lower leg and MTSS
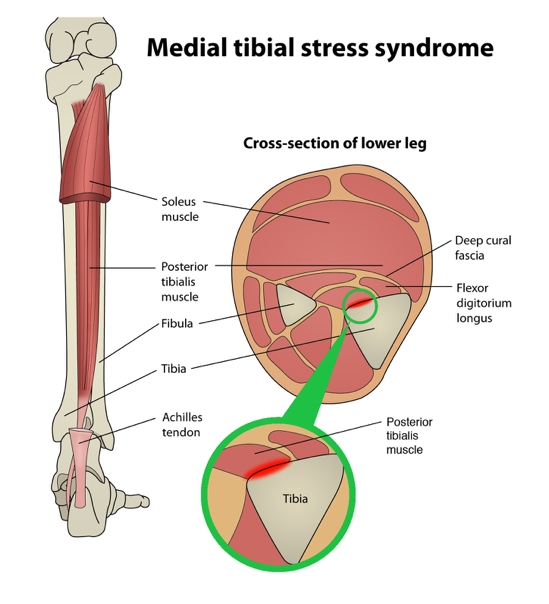
The anatomy of the lower leg makes it unlikely that the posterior leg muscles cause a traction-induced injury to the periosteum of the tibia. Cadaver studies, however, seem to support the theory that repeated or prolonged tension placed on the deep crural fascia by posterior compartment muscle contraction would provide sufficient strain to trigger periostitis and produce pain.
A variation of this tension theory is that the deep crural fascia (DCF) - the though-connective tissue that surrounds the deep posterior compartment muscles of the leg - pulls excessively on the tibia, again causing trauma to the bone. Researchers at the University of Honolulu examined a single leg from five male and 11 female adult cadavers. They confirmed that in these specimens, the muscles of the posterior compartment originated above the portion of the leg that is typically painful in MTSS, and the DCF indeed attached along the entire length of the medial tibia(3).
Doctors at the Swedish Medical Centre in Seattle, Washington wondered if, given the anatomy, could the tension from the posterior calf muscles produce a related strain on the tibia at the insertion of the DCF, and thus be the mechanism of injury(4)?
In a descriptive laboratory pilot study of three fresh cadaver specimens, they found that strain at the insertion site of the DCF along the medial tibia progressed linearly as tension increased in the posterior leg muscles. This confirmed that a mechanism for a tension-induced injury at the medial tibia is plausible. However, studies of bone periosteum in MTSS patients have yet to find inflammatory markers consistently enough to confirm the periostitis theory(5).
Tibial bowing
The second causation theory for MTSS is that repetitive or excessive loading causes a bone-stress reaction in the tibia. The tibia, unable to adequately bear the load, bends during weight bearing. The overload results in micro damage within the bone, and not just along the outer layer. When the repetitive loading outpaces the bone’s ability to repair, localised osteopenia can result. Thus, some consider a tibial stress fracture to be the result of a continuum of bone stress reactions that include MTSS(1).Magnetic resonance imaging (MRI) of the symptomatic leg often shows bone marrow edema, periosteal lifting, and areas of increased bony resorption in patients with MTSS(1,5). This supports the bone-stress reaction theory. Magnetic resonance imaging of an athlete with a clinical presentation of MTSS can also help rule out other causes of lower leg pain such as tibial stress fracture, deep posterior compartment syndrome, and popliteal artery entrapment syndrome.
Risk factors for MTSS
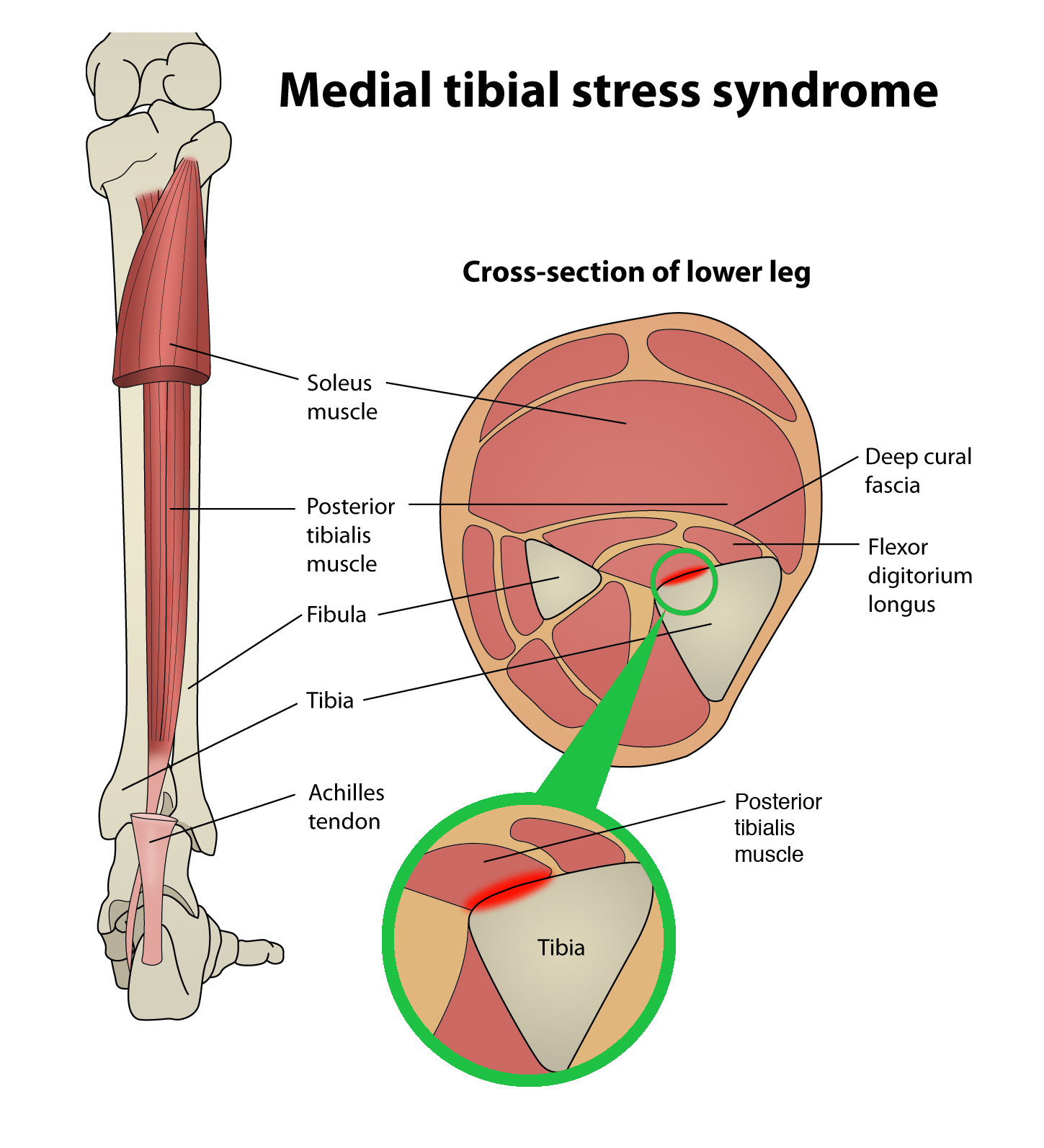
While the aetiology of MTSS is still theoretical, the risk factors for athletes developing it are well determined. A large navicular drop, as determined by the navicular drop test (NDT), significantly correlates with a diagnosis of MTSS(2,5). The NDT measures the difference in height position of the navicular bone, from a neutral subtalar joint position in supported non-weight bearing, to full weight bearing (see figures 2 and 3). The NDT is an indication of the degree of arch collapse during weight bearing. An excursion of more than 10 mm is considered excessive and a significant risk factor for the development of MTSS(5).Figure 2: Navicular drop
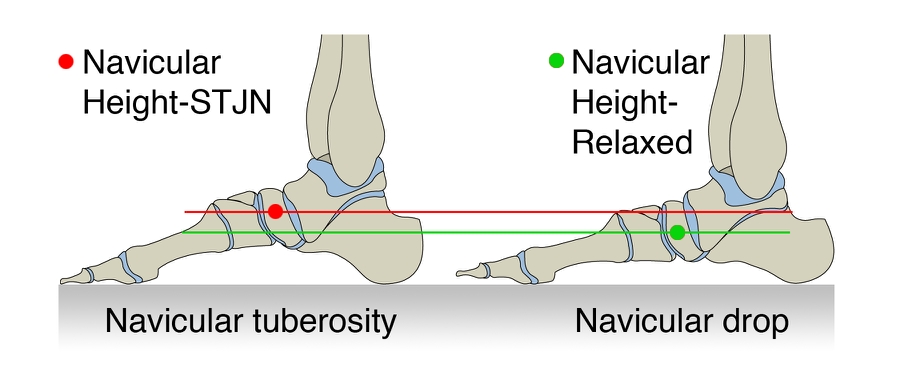
To perform the navicular drop test, have the athlete step forward with the affected leg, and shift weight to that foot. Palpate the tuberosity of the navicular bone and mark it with a pen. Using a ruler or index card, measure the distance from the mark to the floor in this relaxed stance. Next measure the distance with the foot unweighted in the subtalar joint-neutral position (see figure 3).
Figure 3: Palpating medial talar head
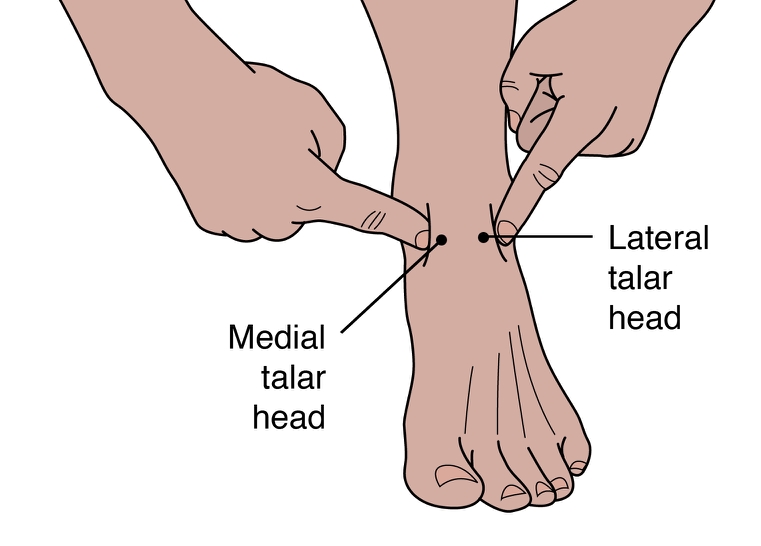
Keeping the foot on the floor in the same position, have the athlete shift weight back to the opposite leg. Palpate the medial talar head and the lateral talar head. Cue athlete to move the tibia slowly side to side until you feel the talus is in a neutral position, with both sides equally protruding. Ask the athlete to maintain this position while again measuring with a ruler or marking on the index card the current position of the mark on the navicular tuberosity. Calculate the difference in the two positions in millimetres. A difference of 10 mm or greater significantly increases the risk of developing MTSS.
Research suggests that athletes with MTSS are found more likely to be female, have a higher BMI, less running experience, and a previous history of MTSS(2,5). Running kinematics for females can differ from males and fit a pattern that is known to leave them vulnerable to anterior cruciate ligament tears and patellofemoral pain syndrome(5). This same biomechanical pattern may also predispose females to MTSS. Hormonal considerations and low bone density are possibly contributing factors in increasing the risk of MTSS in the female athlete as well.
A higher BMI in an athlete likely indicates they have more muscle mass rather than they are overweight. The end result, however, is the same in that the legs bear a significantly heavy load. It is thought that in these instances, the bone growth stimulated by the tibial bowing may not progress rapidly enough, and injury to the bone occurs. Therefore, those with a higher BMI may need to progress their training programs more slowly, to allow for adaptation.
Those with less running experience are more likely to make training errors (often identified by the athlete) as the catalyst for MTSS. These include increasing distance too rapidly, changing terrain, overtraining, poor equipment (shoes), etc. Inexperience may also lead the athlete to return to activity too soon, thus accounting for the higher prevalence of MTSS in those who had suffered MTSS previously. Full recovery from MTSS can take anywhere from six to ten months, and if the cause of injury was not rectified or the athlete returns to training too soon, the chances are good the pain will return(5).
Biomechanical considerations
The NDT is used as a measurable indication of foot pronation. Pronation is a tri-planar movement comprised of eversion at the hindfoot, abduction of the forefoot, and dorsiflexion of the ankle. Pronation is a normal movement, and essential in walking and running. When the foot strikes the ground at the initial contact phase of running, the foot begins to pronate and the joints of the foot assume a loose-packed position. This flexibility helps the foot absorb ground reaction forces (see figure 4).During the loading response phase, the foot further pronates, reaching peak pronation by around 40% of stance phase(6). In mid stance, the foot moves out of pronation and back to a neutral position. During terminal stance, the foot supinates, moving the joints into a closed packed position and creating a rigid lever arm from which to generate the forces for toe off.
Figure 4: The phases of running for the right leg
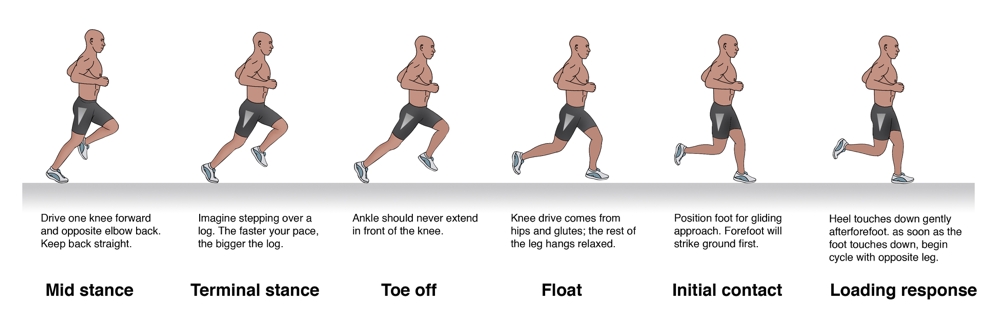
During stance, the foot moves from pronation to supination in order to both absorb and generate forces. Under normal circumstances, peak pronation is reached during the loading response.
Beginning with the loading response phase and throughout the remainder of the single leg stance phase of running, the hip is stabilised, extended, abducted and externally rotated by the concentric contraction of the hip muscles of the stance leg (the gluteals, piriformis, obturator internus, superior gemellus and inferior gemellus). Weakness or fatigue in any of these muscles can result in internal rotation of the femur, adduction of the knee, internal rotation of the tibia, and over-pronation (see figure 5). Overpronation therefore, can be a result of muscle weakness or fatigue. If this is the case, the athlete may have a quite normal NDT, and yet when the hip muscles don’t function as needed, can overpronate.
Figure 5: Stance phase kinetic chain

The relationship of hip, knee, ankle and foot movement in the kinetic chain during the stance phase of running if there is significant weakness or fatigue in the hip muscles.
In a runner who has significant overpronation, the foot may continue to pronate into mid stance, resulting in a delayed supination response, and thus less power generation at toe off. The athlete may attempt two biomechanical fixes here that could contribute to the development of MTSS. Firstly, the tibialis posterior will strain to prevent the over pronation. This can add tension to the DCF and strain the medial tibia. Secondly, the gastroc-soleus complex will contract more forcefully at toe off to improve the power generation. Again, the increased force within these muscle groups can theoretically add tension to the medial tibia through the DCF and possibly irritate the periosteum.
Evaluating the injured athlete
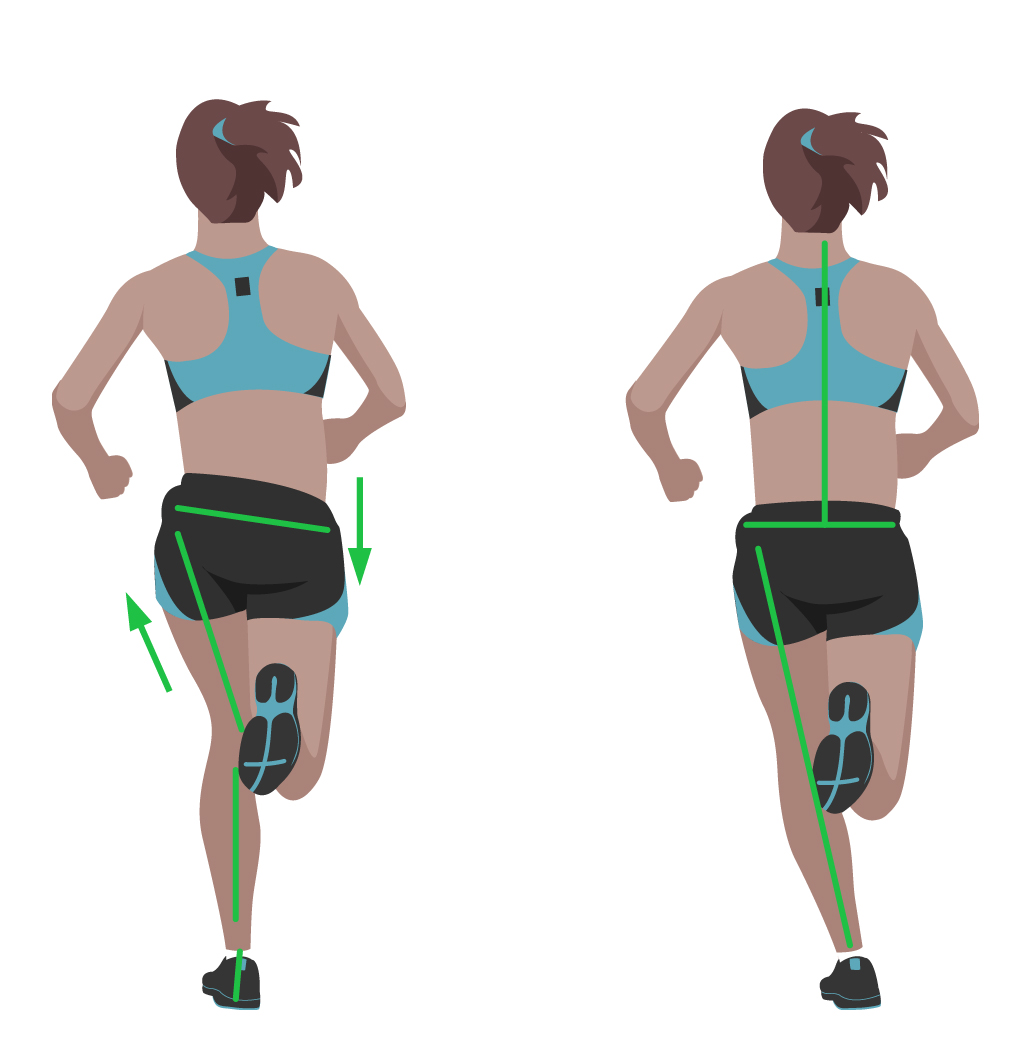
Knowing that overpronation is one of the leading risk factors for MTSS, start your evaluation at the ground and work your way up. First, perform the NDT, noting if the difference is more than 10mm. Analyse the athlete’s running gait on a treadmill, preferably when the muscles are fatigued, as at the end of a training run. Even with a normal NDT, you may see evidence of overpronation in running (see figure 6).Figure 6: Overponation during running

Videotaping your runner while on a treadmill enables you to analyse their gait, frame by frame. Typically, if the runner is overpronating and there is a weakness at the hip joint, at mid stance you will see knee adduction, foot pronation, abduction of the forefoot and a drop of the opposite hip of more than four to five degrees. Some runners may have significant pronation but run with hips level (within five degrees) and minimal knee adduction. In this case, weak tibialis posterior, a tight calf muscle, lax ligaments, or structural deviations may cause the pronation, but the hip tests strong and functions well while running.
Next evaluate the knee. Is it adducted? Notice if the hip is level or if either hip is more than 5 degrees from level. These are indications that there is likely weakness at the hip. Traditional muscle testing may not reveal the weakness; therefore, functional muscle testing is required.
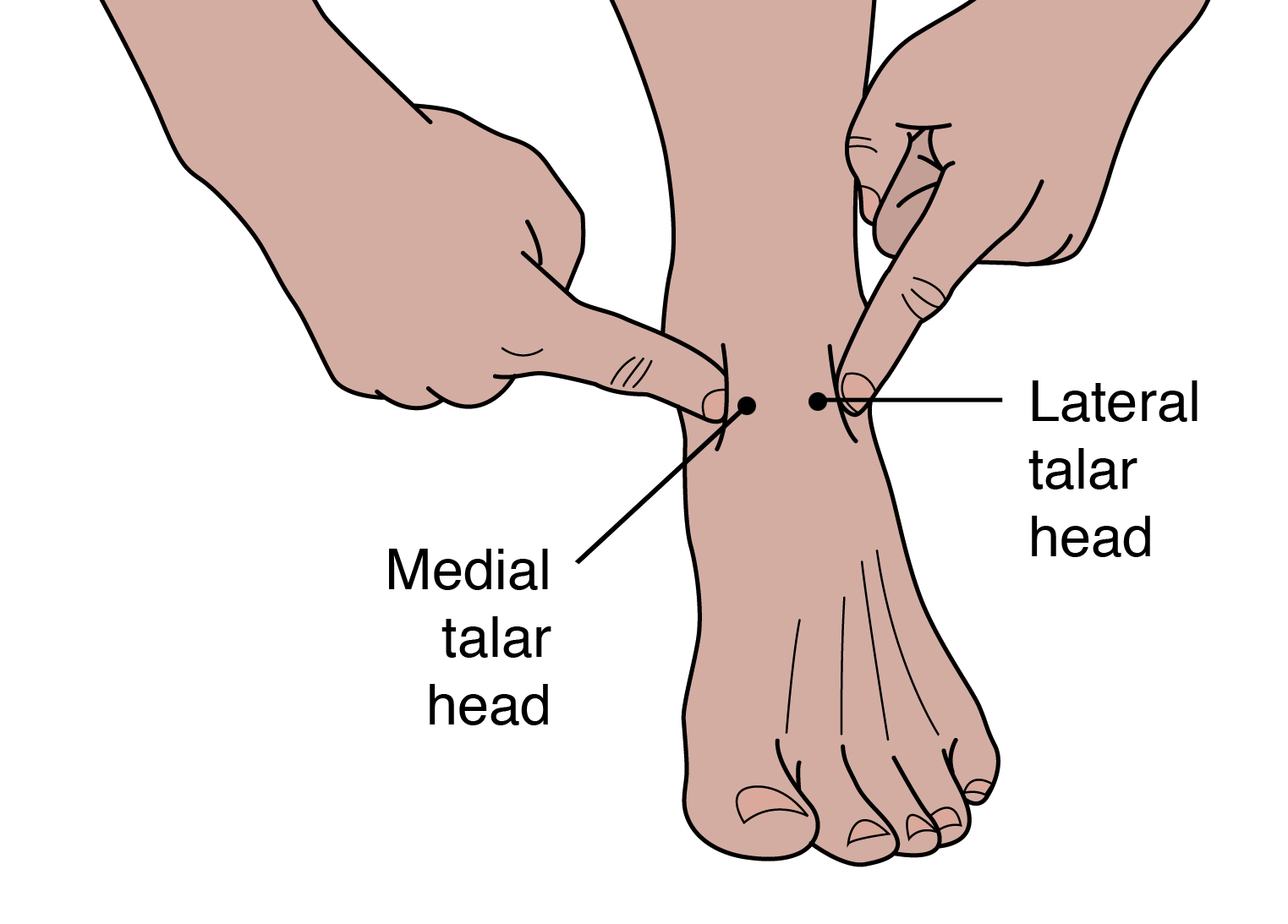
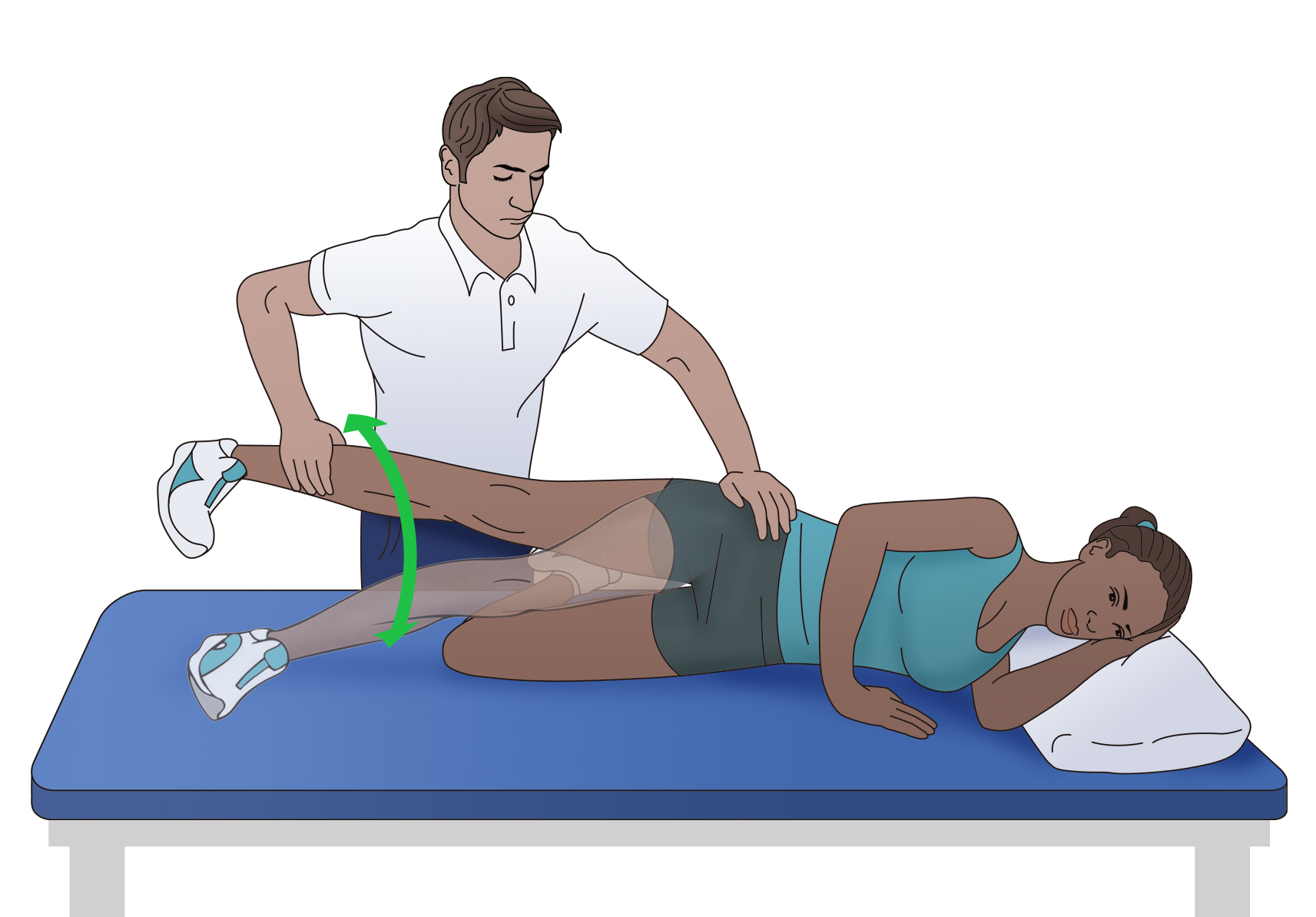
Observe the athlete perform a one-legged squat with arms in and arms overhead. Does the hip drop, the knee adduct and the foot pronate? Test the strength of hip abductors in side lying, with hip in neutral, extended, and flexed, keeping the knee straight (see figure 7). Test all three positions with hip rotated in neutral, and at end ranges of external and internal rotation. Test hip extension in prone with the knee straight and bent, in all three positions of hip rotation: external, neutral and internal. The position where you find the weakness is where you should begin strengthening activities.
Figure 7: Testing hip abduction strength
Test hip abduction in neutral as well as flexion and extension. Perform each test with the hip in external, internal and neutral rotation.
Treat the kinetic chain
If there is weakness in the hip, begin by having the athlete perform isometric exercises in the position of weakness. For instance, if you find weakness in hip abduction with extension, then begin isolated isometrics in this position. Not until the muscles consistently fire isometrically in this position for three to five sets of 10 to 20 seconds should you add movement. Once the athlete achieves this level, begin concentric contractions, in that same position, against gravity. Some examples are unilateral bridging and side lying abduction. Eccentric contractions should follow, and then sport specific drills.Keep in mind if there are other biomechanical compensations, they must also be addressed. If the tibialis posterior is also weak, begin strengthening there. If the calf muscles are tight, initiate a stretching program. Utilise whatever modalities might be helpful. Lastly, consider a stabilising shoe if the ligaments in the foot are over stretched. Using a stabilising shoe for a short time during rehabilitation can be helpful in cuing the athlete to adopt new movement patterns.
Conclusion
The best way to prevent shin pain from MTSS is to decrease the athlete’s risk factors. Ideally, each athlete should have a basic running gait analysis and proper shoe fitting. Include hip strengthening in functional positions such as unilateral stance as part of the strengthening program. Pair inexperienced athletes with a more experienced mentor to ensure proper training, use of equipment, and investigation of pain at onset. They may be more likely to tell a teammate they are feeling pain than a coach or trainer. Progress the running schedule of heavier athletes more slowly to allow adaptation of the bone. Ensure that athletes fully rehabilitate before returning to play because the chances of recurrence of MTSS are high.References
- Am J Sports Med. 2015 Jun;43(6):1538-47
- Br J Sports Med. 2015 Mar;49(6):362-9
- Med Sci Sports Exerc. 2009;41(11):1991-1996
- J Am Podiatr Med Assoc. 2007 Jan;97(1):31-6
- J Sports Med. 2013;4:229-41
- Gait and Posture. 1998;7:77–95

Medial tibial stress syndrome (MTSS – commonly known as shin splints) is not medically serious, yet can suddenly sideline an otherwise healthy athlete. Roughly five percent of all athletic injuries are diagnosed as MTSSAm J Sports Med. 2015 Jun;43(6):1538-47.
The incidence increases in specific populations, accounting for 13-20% of injuries in runners and up to 35% in military recruitsAm J Sports Med. 2015 Jun;43(6):1538-47 Br J Sports Med. 2015 Mar;49(6):362-9. MTSS is defined as pain along the posterior-medial border of the lower half of the tibia, which is present during exercise and (usually) diminishes during rest. Athletes identify the lower front half of the leg or shin as the location of discomfort. Palpation along the medial tibia usually reproduces the pain.
Causes of MTSS
There are two main hypothesised causes for MTSS. The first is that contracting leg muscles place a repeated strain upon the medial portion of the tibia, inducing periostitis – inflammation of the periosteal outer layer of bone. While the pain of a shin splint is felt along the anterior leg, the muscles that arise from this area are the posterior calf muscles (see figure 1). The tibialis posterior, flexor digitorum longus, and the soleus all arise from the posteriormedial aspect of the proximal half of the tibia. Therefore, the traction force from these muscles on the tibia is unlikely to be the cause of the pain typically felt on the distal portion of the leg.A variation of this tension theory is that the deep crural fascia (DCF) – the thoughconnective tissue that surrounds the deep posterior compartment muscles of the leg – pulls excessively on the tibia, again causing trauma to the bone. Researchers at the University of Honolulu examined a single leg from five male and 11 female adult cadavers. They confirmed that in these specimens, the muscles of the posterior compartment originated above the portion of the leg that is typically painful in MTSS, and the DCF indeed attached along the entire length of the medial tibiaMed Sci Sports Exerc. 2009;41(11):1991-1996.
Doctors at the Swedish Medical Centre in Seattle, Washington wondered if, given the anatomy, could the tension from the posterior calf muscles produce a related strain on the tibia at the insertion of the DCF, and thus be the mechanism of injuryJ Am Podiatr Med Assoc. 2007 Jan;97(1):31-6?
In a descriptive laboratory pilot study of three fresh cadaver specimens, they found that strain at the insertion site of the DCF along the medial tibia progressed linearly as tension increased in the posterior leg muscles. This confirmed that a mechanism for a tension-induced injury at the medial tibia is plausible. However, studies of bone periosteum in MTSS patients have yet to find inflammatory markers consistently enough to confirm the periostitis theoryJ Sports Med. 2013;4:229-41.
Figure 1: Anatomy of the lower leg and MTSS
Tibial bowing
The second causation theory for MTSS is that repetitive or excessive loading causes a bone-stress reaction in the tibia. The tibia, unable to adequately bear the load, bends during weight bearing. The overload results in micro damage within the bone, and not just along the outer layer. When the repetitive loading outpaces the bone’s ability to repair, localised osteopenia can result. Thus, some consider a tibial stress fracture to be the result of a continuum of bone stress reactions that include MTSSAm J Sports Med. 2015 Jun;43(6):1538-47.Magnetic resonance imaging (MRI) of the symptomatic leg often shows bone marrow edema, periosteal lifting, and areas of increased bony resorption in patients with MTSSAm J Sports Med. 2015 Jun;43(6):1538-47 J Sports Med. 2013;4:229-41. This supports the bonestress reaction theory. Magnetic resonance imaging of an athlete with a clinical presentation of MTSS can also help rule out other causes of lower leg pain such as tibial stress fracture, deep posterior compartment syndrome, and popliteal artery entrapment syndrome.
Risk factors for MTSS
While the aetiology of MTSS is still theoretical, the risk factors for athletes developing it are well determined. A large navicular drop, as determined by the navicular drop test (NDT), significantly correlates with a diagnosis of MTSSBr J Sports Med. 2015 Mar;49(6):362-9 J Sports Med. 2013;4:229-41. The NDT measures the difference in height position of the navicular bone, from a neutral subtalar joint position in supported non-weight bearing, to full weight bearing (see figures 2 and 3). The NDT is an indication of the degree of arch collapse during weight bearing. An excursion of more than 10 mm is considered excessive and a significant risk factor for the development of MTSSJ Sports Med. 2013;4:229-41.Research suggests that athletes with MTSS are found more likely to be female, have a higher BMI, less running experience, and a previous history of MTSSBr J Sports Med. 2015 Mar;49(6):362-9 J Sports Med. 2013;4:229-41. Running kinematics for females can differ from males and fit a pattern that is known to leave them vulnerable to anterior cruciate ligament tears and patellofemoral pain syndromeJ Sports Med. 2013;4:229-41. This same biomechanical pattern may also predispose females to MTSS. Hormonal considerations and low bone density are possibly contributing factors in increasing the risk of MTSS in the female athlete as well.
A higher BMI in an athlete likely indicates they have more muscle mass rather than they are overweight. The end result, however, is the same in that the legs bear a significantly heavy load. It is thought that in these instances, the bone growth stimulated by the tibial bowing may not progress rapidly enough, and injury to the bone occurs. Therefore, those with a higher BMI may need to progress their training programs more slowly, to allow for adaptation.
Those with less running experience are more likely to make training errors (often identified by the athlete) as the catalyst for MTSS. These include increasing distance too rapidly, changing terrain, overtraining, poor equipment (shoes), etc. Inexperience may also lead the athlete to return to activity too soon, thus accounting for the higher prevalence of MTSS in those who had suffered MTSS previously. Full recovery from MTSS can take anywhere from six to ten months, and if the cause of injury was not rectified or the athlete returns to training too soon, the chances are good the pain will returnJ Sports Med. 2013;4:229-41.
Figure 2: Navicular drop
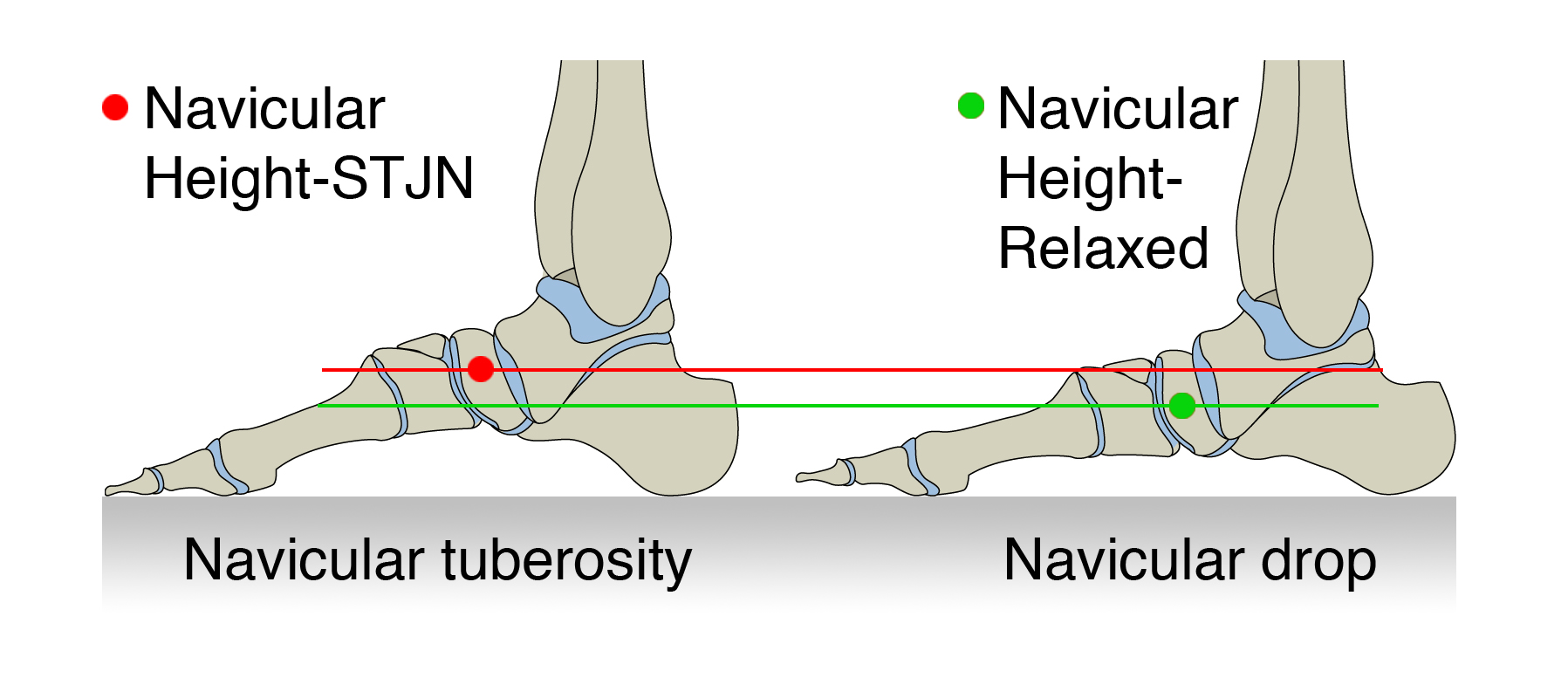
Figure 3: Palpating medial talar head
Biomechanical considerations
The NDT is used as a measurable indication of foot pronation. Pronation is a tri-planar movement comprised of eversion at the hindfoot, abduction of the forefoot, and dorsiflexion of the ankle. Pronation is a normal movement, and essential in walking and running. When the foot strikes the ground at the initial contact phase of running, the foot begins to pronate and the joints of the foot assume a loose-packed position. This flexibility helps the foot absorb ground reaction forces (see figure 4).
Figure 4: The phases of running for the right leg
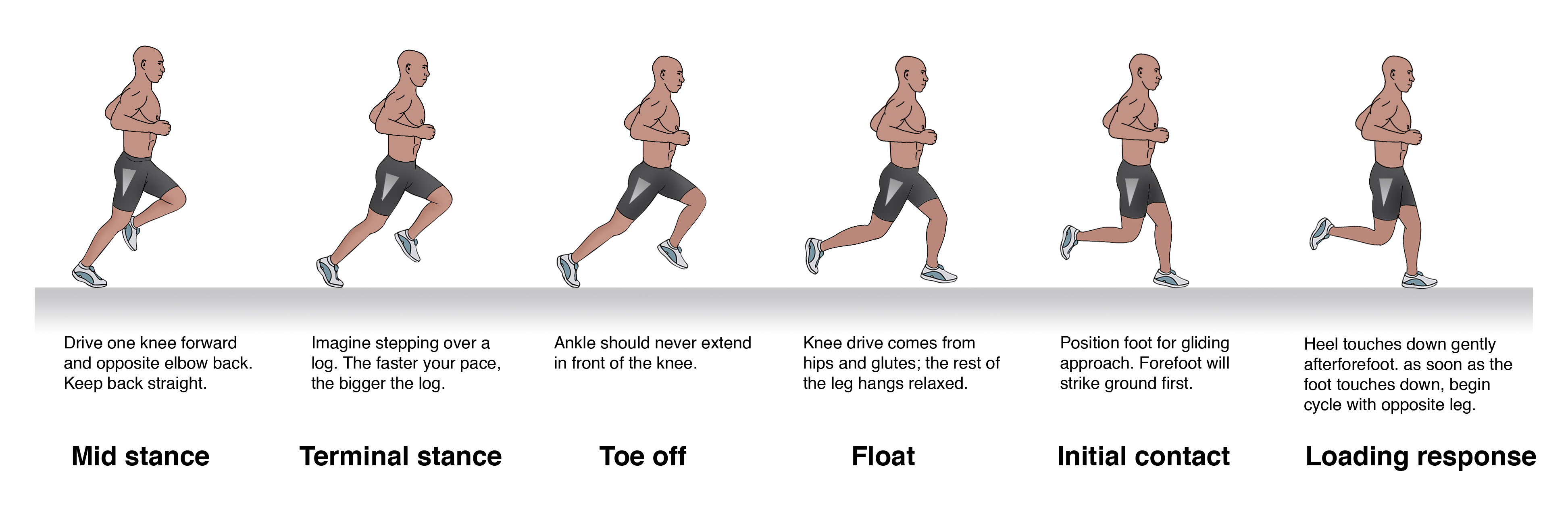
During the loading response phase, the foot further pronates, reaching peak pronation by around 40% of stance phaseGait and Posture. 1998;7:77–95. In mid stance, the foot moves out of pronation and back to a neutral position. During terminal stance, the foot supinates, moving the joints into a closed packed position and creating a rigid lever arm from which to generate the forces for toe off.
Beginning with the loading response phase and throughout the remainder of the single leg stance phase of running, the hip is stabilised, extended, abducted and externally rotated by the concentric contraction of the hip muscles of the stance leg (the gluteals, piriformis, obturator internus, superior gemellus and inferior gemellus). Weakness or fatigue in any of these muscles can result in internal rotation of the femur, adduction of the knee, internal rotation of the tibia, and over-pronation (see figure 5). Overpronation therefore, can be a result of muscle weakness or fatigue. If this is the case, the athlete may have a quite normal NDT, and yet when the hip muscles don’t function as needed, can overpronate.
Figure 5: Stance phase kinetic chain
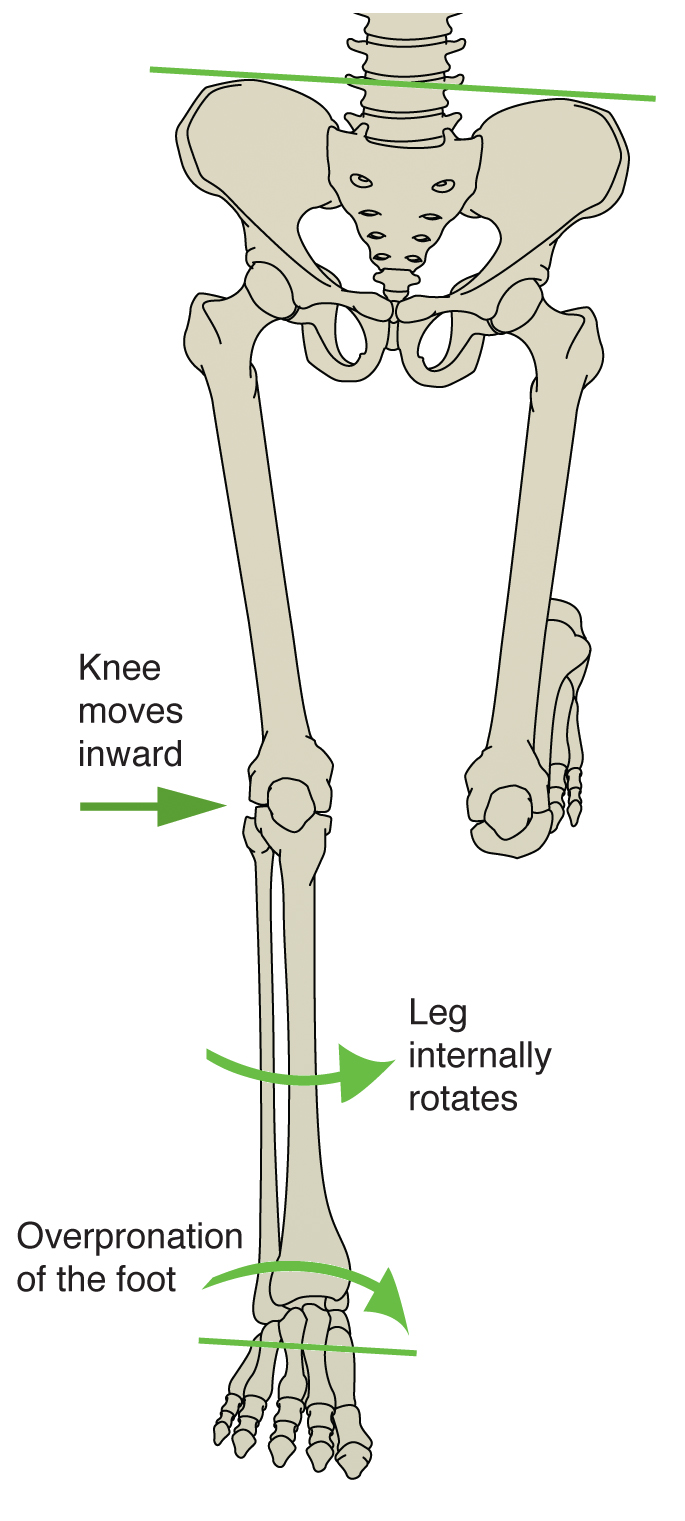
In a runner who has significant overpronation, the foot may continue to pronate into mid stance, resulting in a delayed supination response, and thus less power generation at toe off. The athlete may attempt two biomechanical fixes here that could contribute to the development of MTSS. Firstly, the tibialis posterior will strain to prevent the over pronation. This can add tension to the DCF and strain the medial tibia. Secondly, the gastroc-soleus complex will contract more forcefully at toe off to improve the power generation. Again, the increased force within these muscle groups can theoretically add tension to the medial tibia through the DCF and possibly irritate the periosteum.
Evaluating the injured athlete
Knowing that overpronation is one of the leading risk factors for MTSS, start your evaluation at the ground and work your way up. First, perform the NDT, noting if the difference is more than 10mm. Analyse the athlete’s running gait on a treadmill, preferably when the muscles are fatigued, as at the end of a training run. Even with a normal NDT, you may see evidence of overpronation in running (see figure 6).
Figure 6: Overponation during running
Next evaluate the knee. Is it adducted? Notice if the hip is level or if either hip is more than 5 degrees from level. These are indications that there is likely weakness at the hip. Traditional muscle testing may not reveal the weakness; therefore, functional muscle testing is required.
Observe the athlete perform a one-legged squat with arms in and arms overhead. Does the hip drop, the knee adduct and the foot pronate? Test the strength of hip abductors in side lying, with hip in neutral, extended, and flexed, keeping the knee straight (see figure 7). Test all three positions with hip rotated in neutral, and at end ranges of external and internal rotation. Test hip extension in prone with the knee straight and bent, in all three positions of hip rotation: external, neutral and internal. The position where you find the weakness is where you should begin strengthening activities.
Figure 7: Testing hip abduction strength
Treat the kinetic chain
If there is weakness in the hip, begin by having the athlete perform isometric exercises in the position of weakness. For instance, if you find weakness in hip abduction with extension, then begin isolated isometrics in this position. Not until the muscles consistently fire isometrically in this position for three to five sets of 10 to 20 seconds should you add movement. Once the athlete achieves this level, begin concentric contractions, in that same position, against gravity. Some examples are unilateral bridging and side lying abduction. Eccentric contractions should follow, and then sport specific drills.Keep in mind if there are other biomechanical compensations, they must also be addressed. If the tibialis posterior is also weak, begin strengthening there. If the calf muscles are tight, initiate a stretching program. Utilise whatever modalities might be helpful. Lastly, consider a stabilising shoe if the ligaments in the foot are over stretched. Using a stabilising shoe for a short time during rehabilitation can be helpful in cuing the athlete to adopt new movement patterns.
Conclusion
The best way to prevent shin pain from MTSS is to decrease the athlete’s risk factors. Ideally, each athlete should have a basic running gait analysis and proper shoe fitting. Include hip strengthening in functional positions such as unilateral stance as part of the strengthening program. Pair inexperienced athletes with a more experienced mentor to ensure proper training, use of equipment, and investigation of pain at onset. They may be more likely to tell a teammate they are feeling pain than a coach or trainer. Progress the running schedule of heavier athletes more slowly to allow adaptation of the bone. Ensure that athletes fully rehabilitate before returning to play because the chances of recurrence of MTSS are high.Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










