You are viewing 1 of your 1 free articles
Back in action: causes and remedies for low back pain in runners

Running is one of the most popular sporting activities worldwide. Still, it carries a high injury risk in both amateur and professional athletes, with up to 85% of runners sustaining a running-related injury (RRI) per year(1). Approximately 80% of these are overuse injuries due to repeated single-plane movement(2,3). Recurring one-dimensional activity – movement in the sagittal plane in this instance – can cause muscle weakness and imbalance. When these dysfunctions prevent the legs from absorbing the ground reaction forces as they should, the strain can migrate up the kinetic chain to the lumbar spine(2,4).
Up to 13.6% of runners in the US experience LBP(5). Those runners most affected by LBP typically have(6):
- A history of running for six years or more.
- A BMI greater than 24.
- Reduced hip flexion.
- Low back stiffness.
- Poor hamstring function.
- A leg length discrepancy.
- Excessive height.
- Low aerobic endurance.
The cause of LBP in most runners (90%) is non-specific and mechanical(7). This diagnosis means a specific pathology, such as a herniated disc, compressed nerve, or degeneration of a spinal disc or joint, isn’t the cause of pain.
There are many structures in the back with nociceptive properties, meaning they have sensors that detect noxious stimuli or perceived threats to the body. Sometimes, these structures become overly sensitized and require less input to trigger nerve impulses to the brain. The brain perceives these highly charged impulses as pain. As the nerves become hyper-sensitized, the impulse signals appear to increase in magnitude, producing a greater response from a somewhat innocuous stimulus (see figure 1). For example, a sensitized system will sound the alarm to send in the fire brigade to put out a candle flame when a puff of air will do.
The back is a robust and stable structure that requires significant trauma to exhibit real damage. Therefore, runners with LBP likely suffer from over sensitization because the tissues cannot handle the repetitive load, rather than a severe pathology. Findings on imaging exams may be incidental in runners who meet the profile of those who suffer from non-specific mechanical LBP. The clinician’s job is to figure out the reason for the added strain at the low back and prescribe a program to calm the sensitivity, stabilize the trunk, improve lower body strength, and correct running biomechanics.
Figure 1: Spinal sensitization
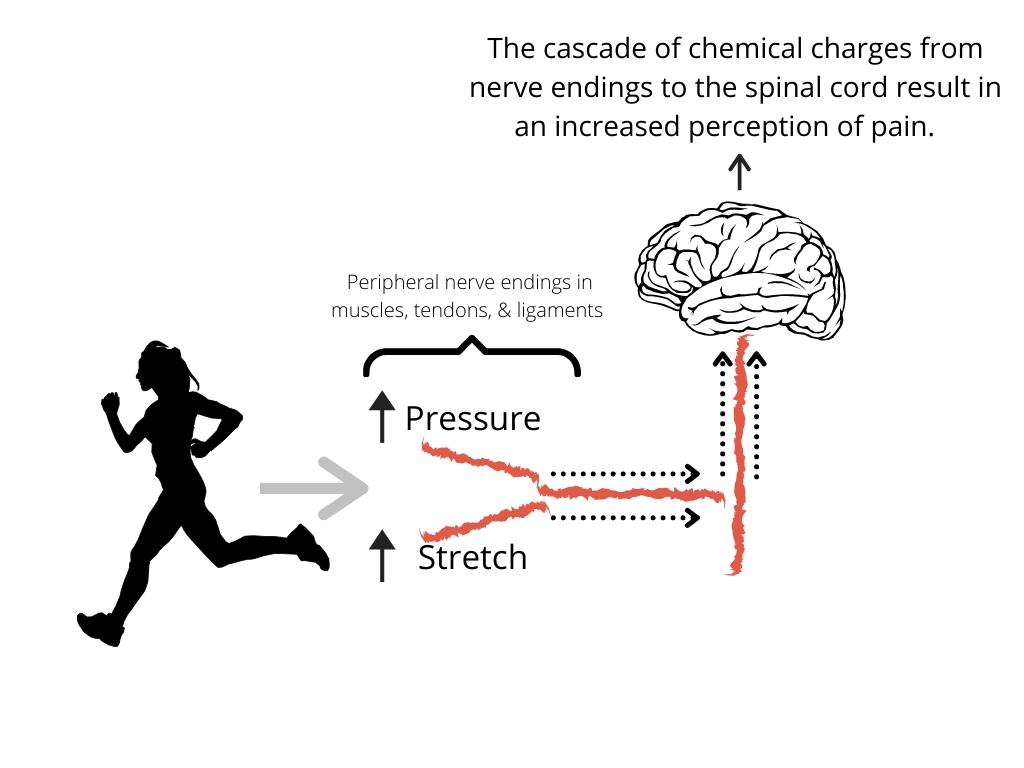
Schematic diagram showing the sensitization process that contributes to low back pain in runners
ASSESSMENT STRATEGIES
Athlete perceptionsBegin an evaluation with a subjective history of training load, including volume, intensity, schedule, and type of training. This background information will reveal the athlete’s external and internal stresses, such as a lack of sleep and short recovery periods, which contribute to LBP. To assess these psychosocial aspects objectively, use a validated outcome measure such as the Orebro Screening Questionnaire (to identify recurrent risk), Pain Catastrophizing Scale (to identify negative thoughts), or the Tampa Scale of Kinesiophobia (to assess fear avoidance). Indeed, runners with LBP have more fear-avoidance beliefs than control groups(5).
If the athlete has negative thoughts about their LBP, their fear avoidance could foster dysfunctional movement patterns and delay recovery. Underlying psychosocial issues may also contribute to guarded movement patterns. Identifying and addressing these issues is an essential component of a therapeutic intervention. Education and empathy is the first aspect of treatment of pain patients.
Movement observations
In addition to evaluating the runner’s perceptions and mental wellbeing, conduct a thorough physical screening for any red flags that might signal a more serious pathology. Up to 80% of people with acute LBP have at least one red flag despite not having a severe diagnosis(8,9). However, be mindful of any observed neurological changes. The physical assessment should also include measures of strength, range of motion, and movement patterns – particularly:
- Postural control of the trunk and upper body.
- Balance and stability of the lower limbs.
- Muscular control during the shock absorption phases of running and jumping.
- Energy generation associated with forward and upward propulsion.
- Control of directional changes and center of mass movement(10).
Key single-leg tests
The hallmarks of running are the float and single-leg stance phases. Note that both feet are never on the ground at the same time. Each leg is airborne twice during each gait cycle and the ground contact time of the single-leg decreases as speed increases(11). Therefore, stability in single-leg support is vital.
Muscle activity is heightened at the transition from the swing to the stance phase (i.e., the preparation for ground contact and foot strike). The legs use this increased activation to absorb the forces on landing and reduce the transmission of these forces up the kinetic chain to the pelvis and lumbar spine(12).
There are several ways to test the body’s functional response to this phase of running. A typical reaction to these movement tests is symmetry, strength, and control. Compensatory, painful, or limited ranges of movement suggest muscle imbalances and instability. Important tests to assess single-leg functional strength include:
- Single-leg stand: View the runner from the front and the back as they transition to single-leg standing. Look for a contralateral hip drop or pelvic tilt, and assess femur, knee, and ankle alignment. The runner should stand for a minimum of 20 seconds on each side without wavering.
- Single-leg squat: The load here is similar to that applied to the muscles when running but without the impact of landing. Therefore, the runner should complete multiple repetitions and avoid a contralateral hip drop, flexion through the lumbar spine, hip adduction, and valgus knee positioning.
- Single-leg hop: The hop element comes closer to the impact experienced when running and assesses the same kinematic responses as the single-leg squat above.
Lumbar movement and control tests
Next, assess lumbar movement and control. Use pelvic tilts to measure lumbar-pelvic dissociation. In other words, can the athlete move these two regions independently of each other? Segmental movement between the spine and pelvis reduces vertebral stiffness and promotes shock absorption by the intervertebral discs instead of the muscles and joints.
As the runner increases speed, their pelvis tilts forward to lower their center of mass and maximize the horizontal propulsion force. If the runner tried to accelerate while remaining fully upright, they would fall backward due to the ground reaction force. Therefore, adequate pelvic mobility is necessary for effective acceleration(10).
Pelvic tilts also teach the athlete how to achieve a neutral spine position, with the pelvis tilted neither excessively forward nor back. Adopting a neutral spine position promotes successful and maximal recruitment of the core muscles(13). First, test pelvic tilts in a quadruped position. This posture makes it easier to initiate the movement by performing a cat/cow exercise (see figure 2). Next, progress them to a seated position where there is more load on the lumbar spine. Finally, assess their ability to perform a pelvic tilt in a split stance position. This posture imitates the functional posture when running. The runner should be comfortable alternating between an anterior and posterior pelvic tilt without tightness or pain.
Figure 2: Pelvic tilt test
A) B)
B) 
A) Four-point kneeling cat stretch bringing the spine into extension.
B) Four-point kneeling cow stretch with the spine in flexion.
STRENGTH DEMANDS OF RUNNING AND TREATMENT STRATEGIES
Running produces a ground reaction force of up to five times the body’s weight, and an internal compressive force to the leg of approximately 10 to 14 times bodyweight(14). Even with the absorption of these forces by the legs, the lumbar spine still experiences forces between two and five times bodyweight with each foot strike.Lower limb strengthening programs effectively reduce the load and pain experienced at the lumbar spine(5). Stronger muscles are better able to absorb ground reaction forces(15). Runners with non-specific LBP showed a 72% improvement in symptoms after a 16-week strengthening program(16). A runner’s strength and conditioning program should build the athlete to achieve greater than or equal to 70% one-repetition maximum for 3-6 sets of 6-10 repetitions, with 90% to 100% symmetry between legs(17).
Core musculature
The core muscles stabilize the trunk and pelvis and help transfer forces from the lower limbs to the trunk and upper body(18). However, the experience of pain impairs and inhibits muscle contraction and function. Back pain also produces atrophy, fatigue, and delayed activation of the core muscles(19,20,21,22). Within 24 hours of a single LBP episode, the multifidus’ cross-sectional area reduces by 20%. Therefore, while core dysfunction might not be the direct cause of the LBP, core training is essential for any runner with LBP.
Pilates-based core programs for LBP have the most positive effect on pain intensity and physical function than other exercise types(23). Begin Pilates-based core work in supine to eliminate gravity and ensure engagement of the deep core muscles, rather than accessory ones. Progress through closed-chain exercises, followed by open-chain, and incorporate spinal movement in these positions before implementing functional running-specific drills (see figure 3).
Figure 3: Examples of staged core exercises
A) B)
B) 
- A) Closed chain hip twist – In supine with feet on the floor, keep the pelvis neutral and hips flat on the floor and twist at the pelvis moving knees side to side.
- B) Open chain scissors – Keeping a neutral spine, flex one hip and knee up to table-top position. Stabilize pelvis as you alternate legs in this position with legs moving together as a pair of scissors would.
C)
 D)
D) 
- C) Open chain swimming – Assume a neutral pelvis in a quadruped position. Stabilize core and alternate extending arms and legs slowly with control.
- D) Incorporating spinal movement shoulder bridge with ball – In supine, assume a neutral pelvis with feet on the floor, knees bent, and squeeze a soft ball between the knees. Bridge, keeping pelvic control, and extend one leg into a single-leg bridge. Slowly and with control, alternate extended legs while in the bridge position.
Hamstrings and quadriceps
Runners with chronic non-specific LBP have reduced knee extensor strength, which may contribute to greater loads experienced at the lumbar spine(5). In late swing phase, the quadriceps work concentrically and become dominant to produce knee extension. After initial contact, the quadriceps work eccentrically and play an important role in shock absorption as the limb advances (see figure 4).
In late swing phase, the hamstrings contract eccentrically to control momentum of the tibia and prevent knee hyperextension. In stance, they assist with hip extension over the foot. As the quadriceps and hamstrings are both bi-articular muscles (crossing two joints), they transfer energy between these joints. Simultaneous coordination and sufficient strength are essential for the biomechanics to work smoothly. Any dysfunction in this mechanical pattern can place excessive strain on the muscles and joints of the lumbar spine.
Figure 4: Anatomy of a runner

Gluteal muscles
The gluteal muscles are integral to running biomechanics, and their weakness can contribute to LBP (24). Although the gluteus maximus is the driver in hip extension and power production, the medius and minimus are essential for stabilizing the hip joint during running(25). A lateral gluteal weakness can increase the peak impact vertical ground reaction force and impair the body’s ability to absorb this force, increasing the stress on the lumbar spine(26).
To check for lateral gluteal muscle weakness, complete these tests and compare each side:
- Resisted side-lying hip abduction.
- Active and passive range of motion of side hip abduction; a difference of more than 15 degrees suggests an active lag and weakness.
- Side abduction to fatigue.
- Single-leg glute bridge to fatigue – aim for 25 repetitions on each side.
Exercises to rehabilitate the weakness:
- Lateral step-ups.
- Single-leg squats.
- Pelvic drop exercise.
- Skater squats (squat on one leg with the other leg diagonally out behind you)(25).
Calf muscles
The calf muscles need to absorb body weight in a quick, reactive manner. They also need the endurance to withstand this repetitive load over long run durations. Running also requires the calf muscles to execute an efficient stretch-shortening cycle (SSC). This phenomenon occurs when the active muscle lengthens and then immediately contracts and shortens. In the calf, the SSC relies on energy storage and release by the Achilles tendon, and strong muscular contractions from the triceps surae(27). A defect in the SSC can cause a reduction in the efficiency of movement and alter power production, giving way to muscle imbalances and strain.
Plyometric training is often underused in running training plans. However, it is essential for the development of an efficient SSC to drive the runner. After all, running is essentially lots of single-leg hops. When a runner lacks power and running economy, overworked calf muscles can alter lower limb biomechanics. Any inefficiency here results in straining further up the kinetic chain to compensate, including at the lumbar spine.
An effective calf loading protocol to ensure maximum power performance for the runner should consist of isometric, isotonic, and plyometric based exercises (see table 1)(27):
| Isometric exercises | Isotonic exercises | Hops |
|---|---|---|
| Seated heel raises 5 x 45 seconds, pushing toes against the ground as strongly as possible, bodyweight only. | Standing heel raises 2 x 25 reps. | 3 x 30 double leg hops (DL). |
| Seated heel raises 3 x 8 reps at 80% of 6RM. | 3 x 5 DL hops forward/backwards. | |
| 3 x 5 DL hops on to a step. | ||
| Repeat all of the above but with single-leg hops on each leg. |
Summary
- Running related injuries are predominantly due to overuse and affect the lower limbs, pelvis, and lower back. Ninety percent of LBP in runners is classified as non-specific LBP. Long-time runners and those with altered kinematics have a greater risk of experiencing LBP
- Treatment should first identify the athlete’s perceptions and psychosocial factors that may contribute to pain, such as anxiety, stress, fear-avoidance, training demands, and recovery.
- Movement observations should analyze the runner’s movement during functional tasks. Conduct further tests to identify biomechanical and strength deficits. Deficiency in lower limb strength or movement patterns can create an excessive force transfer to the lumbar spine.
- Single-leg tests, including single-leg stand, single-leg squat, and single-leg hopping, are essential because they simulate the postural control needed when running.
- Lumbar movement and control tests include evaluation of pelvic tilting in various positions and with core engagement.
- Begin rehabilitation for LBP by improving the effectiveness of core muscle activation and strength. This foundation is essential before adding strength and conditioning elements.
- Strength training should ensure the runner can meet the demands of their runs, with attention to the strength of the hips, quadriceps, hamstrings, and calf muscles. Adequate strength ensures the proper absorption of ground reaction forces and lessens strain on the lumbar spine.
- Appreciate the gluteal muscle’s role in unilateral stance and power development and be sure to train each effectively. Strengthen the lateral gluteal muscles with exercises such as side-lying abduction, single-leg bridges, hip drops, and lateral step-ups.
- Calf muscle loading should include a combination of isometric, isotonic, and plyometric-based exercises to train for the shock absorption levels experienced when running.
References
- Int J Sports Phys Ther. 2012;7:58.
- Overuse 80%. Med Sci Sports Exerc. 2000;32(9):1635–41.
- Int J Sports Med. 2017;38:776-780.
- Affect pelvis, Lx. Sports Med. 2012;42:891–905.
- Med Sci in Sport & Exerc. 2017;49(1):2374-2384.
- BMC Musculoskeletal Disorders. 2020;21:343.
- Rheumatol Int. 2019;39(4):619–26.
- 2018;391(10137):2356-2367.
- Eur Spine J. 2018;27(11):2791–803.
- Gait and posture. 1998;7:77-95.
- AAOS Instructional Course Lectures. 1995;44:497-506.
- J Biomech. 1994;27(4):501-508.
- Neurology and Urodynamics. 2001;20(1):31-42.
- Med Sci Sports Exerc. 2004;36(5):845-849.
- Br J Sports Med. 2019. 10.1136/bjsports-2019-100840.
- BMJ Open Sport Exerc Med 2015;1:000050. doi:10.1136/bmjsem-2015-000050.
- Br J Sports Med.2019. 10.1136/bjsports-2019-101168.
- Strength & Cond J. 2000.22:50-61.
- 1994;19:165-172.
- 1991;17:1179-1185.
- 1993;18;568-574.
- 2003;28:1593-1600.
- Br J Sports Med. 2020;54:1279-1287.
- Eur Spine J. 2016;25:1258-1265.
- 2020; 42(1):60-66.
- Access J Sports Med.2009;8:284-288.
- Phys Ther in Sport. 2019;40:107-116.
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.