You are viewing 1 of your 1 free articles
Uncommon injury: Scapular body fracture

Most scapular fractures in the human body occur as a result of a high-energy impact, such as a motor vehicle accident(1). Scapular fractures represent just 1% of all fracture injuries likely due to the relatively deep location of the scapula body and surrounding musculature(2). When it comes to sport, a scapular fracture is very rare. In one study, that accumulated data for 7920 player participation hours across a range of sports and 306 players, the reported rate of fractures of the scapula ranged from 1 to 10 injuries per ten thousand hours of sports participation(3).
High-risk sports
As might be expected, players in sports that involve collisions – either accidental or intentional – such as rugby and soccer are at increased risk of scapular fracture. Elite rugby players may be especially at risk as they suffer frequent high-energy collisions. During a tackle or collision, a player experiences impact forces over double their body weight, around 400+lbs(4).Most shoulder injuries are due to acute trauma(5). These injuries occur from both contact and non-contact mechanisms. Athletes participating in American football, wrestling, and water skiing tended to suffer injury as a result of forceful rotation movements. In contrast, ice hockey, boxing, and badminton injuries happen due to forceful swinging movements. Fatigue fractures are rare. Some mechanisms for repetitive stress fractures include pitching in baseball players, an extended season of batting in cricket players, and jogging with hand weights in runners.
Injury mechanism and fracture type
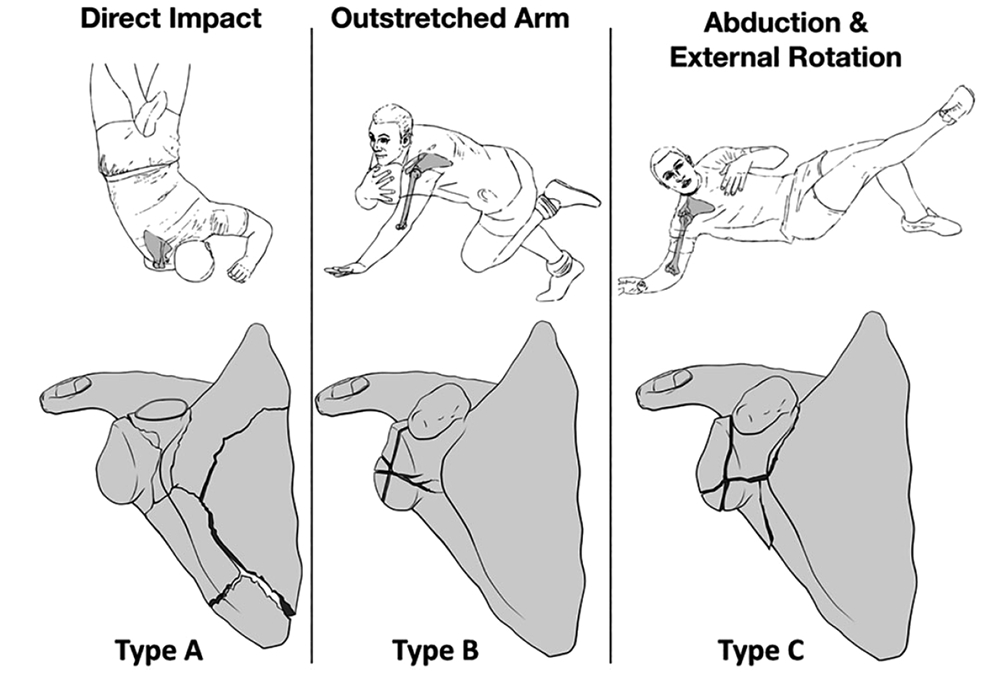
The scapular is a large structure with various regions and bony protrusions, which experience different loading forces depending on the movement of the arm (see figure 1). This varied loading means that different types of scapular fractures occur at each location. The system of scapula fracture classification is based on the mechanism and site of injury (see figure 2 and table 1)(4).Figure 1: Regions of the scapula
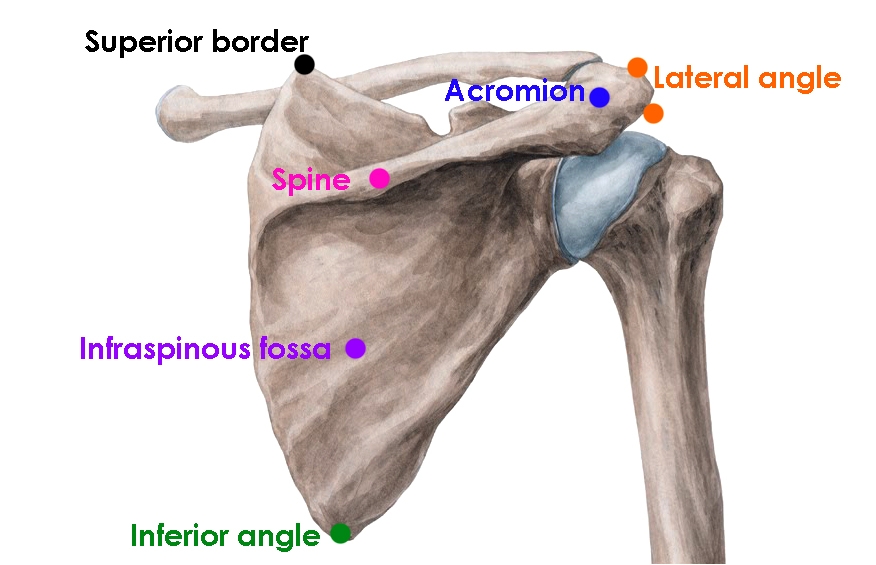
Figure 2: Scapular fracture classification*(4)
*Used with permission
| Type A: Extra-articular fracture involving the scapula neck and body. |
| Type B: Intra-articular glenoid fracture involving more than 25% of the articular surface. |
| Type C: Intra-articular glenoid fracture extending into the base of the coracoids. |
Though rare, a fatigue fracture of the scapular body is occasionally observed and only ever documented in athletes(6). The mechanism of a scapular body fatigue fracture appears to involve repetitive trauma across the bone (as a result of cumulative muscular contractions), which results in microfractures occurring in the scapular body(7). The more subtle nature of this type of fracture makes a diagnosis rather more difficult.
Diagnosis
With so few cases of sports-related scapular fracture in the literature, there is no universally agreed protocol for diagnosis of this type of injury. However, some typical characteristics are(8):- A sudden onset of pain, usually localized across the shoulder blade or at the top of the shoulder – but which may also be diffuse - and which worsens with time. (NB: note too that, although extremely rare, a fatigue fracture of the scapula likely presents with a much more gradual onset of pain.
- Pain that worsens with arm movement or deep inhalation.
- Pain that is severe when the athlete attempts to raise the arm overhead.
- Severely limited range of motion, particularly abduction.
- A grinding sensation during movement.
- Swelling, tenderness, and bruising in the superior scapula region, or on the top of the shoulder overlying the coracoid and acromion processes.
- When viewed from the side, a slightly flattened or deformed appearance compared to the unaffected side.
In addition to noting the presenting symptoms, clinicians should also obtain a detailed injury history from the athlete. A previous shoulder injury is a significant risk factor for further injury(4). In a 2019 English review of 11 athletes with scapular fractures, four experienced a previous shoulder injury(4). These were:
- One case of an ACJ injury (which required reconstruction), followed several years later by a separate scapula fracture, which required surgical fixation.
- One example of a previous anterior labral stabilization.
- Two instances where the athletes had had previous Latarjet procedures.
Imaging
X-ray imaging is the first diagnostic choice for suspected scapular fracture. These images often provide the clinician with definitive confirmation of a scapular fracture and the fracture type. However, type B and C fractures are not always identifiable using X-ray imaging alone(4). Therefore, radiographs cannot rule out a scapular fracture. The preferred diagnostic tool for type B and C injuries caused by an outstretched arm or a combination of abduction and external rotation is either an MRI or CT scan (see figure 3).Figure 3: Comparison of X-ray vs. CT imaging(9)
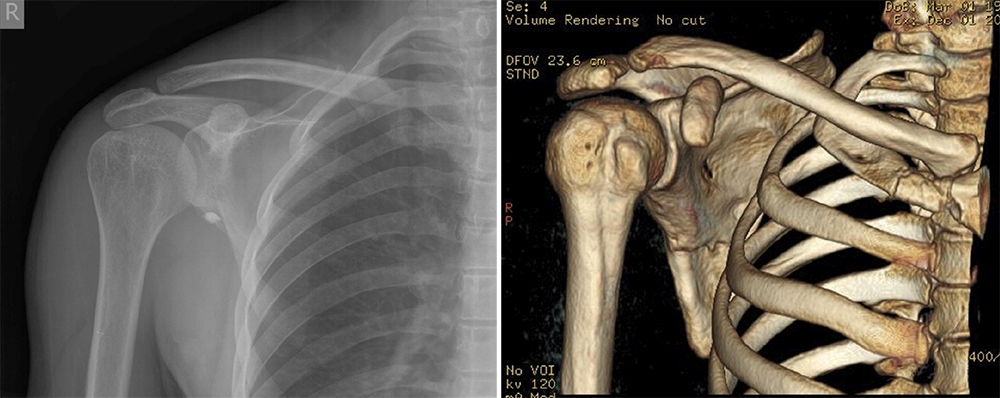
Anteroposterior X-ray image left; 3-dimensional colored CT image right. The fracture – resulting from a type C abduction and external rotation event – is more clearly seen by CT scanning.
If the injury mechanism is suspected to be a fatigue fracture, X-ray imaging is unlikely to provide a confirmatory diagnosis. While a radiograph will usually detect abnormalities such as a bony callus formation in the region of the injury, it is unlikely to catch a microfracture, even several weeks or months after the onset of symptoms. Magnetic resonance imaging and CT imaging are the preferred choices for a suspected fatigue fracture.
Treatment protocols
Due to the rarity of this injury, there are no standard rehab protocols for returning athletes to sport(10). However, the nature and mechanism of the injury are thought to provide useful guidelines as to the best treatment options. Conservative management suffices for many scapular body fractures (2,7,11). The vast majority of them involve only minimal displacement – thanks to the thick, strong support provided by the surrounding muscle mass(6).Conservative management appears to have outcomes equal to or better than surgical management. A study comparing two groups of 31 patients, who were treated either operatively or non-operatively for scapular fracture, found no significant difference in rates of union, range of motion, or ability to return to work between the groups (11). If surgery is needed, it requires a fair amount of muscle detachment, which necessitates a longer recovery. For this reason, surgical repair should be considered only as a last resort.
Conservative rehab
The typical rehab protocol for conservative treatment is as follows (time frame two to six months(4)):- Immobilize using a sling and swathe for comfort (for up to six weeks).
- Begin a progressive range of motion exercises as soon as the pain subsides.
- Start progressive loading against resistance once pain free, concentrating on developing the maximum range of motion – for example, using Therabands.
- Introduce heavier and more sports-specific loading when movements are pain-free, and follow up imaging confirms union is taking place.
- Considered a return to sport once the athlete recovers a full range of motion, and bilateral strength symmetry and no pain is present.
Even with widely displaced scapular body fractures, this treatment approach is likely to produce reliable fracture healing with restored shoulder function(12).
When surgery is needed
Injuries sustained via an outstretched arm (type B) typically lead to Ideberg type 1B or type 2 fracture of the posterior glenoid, and are associated with posterior labral tears. In contrast, injuries resulting from abduction plus external rotation (type C) may typically involve an anterior fracture, which includes the coracoid base(4). This underlines the importance of confirming (if possible) the injury mechanism. If confirmed by imaging, surgical fixation will be indicated for these, unstable fractures of the scapular neck, and significantly displaced apophyseal fractures. A conservative management approach in these injuries is unlikely to be successful, resulting in non-union, malunion, and longer-term disability/poor functionality of the shoulder(12).References
- J Trauma. 1980;20(10):880-883.
- J Am Acad Orthop Surg. 1995;3(1):22-33
- J Sci Med Sport. 2015;18(5):529–33
- Orthop J Sports Med. 2019 Dec 2;7(12):2325967119887388
- Curr Rev Musculoskelet Med. 2019 Mar; 12(1): 13–23
- HSSJ (2018) 14:328–332
- Skelet Radiol. 1982;9(1):27–32
- Sports Health. 2012 Nov; 4(6): 502–503
- Annals of Medicine and Surgery 4 (2015) 235e237
- J Bone Joint Surg Br Vol. 1984;66(5):725–31
- Clin Orthop Relat Res. 1991;(269):174–180
- Operative Orthopaedics. Philadelphia: JB Lippincott; 1988:197–202
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










