You are viewing 1 of your 1 free articles
Uncommon injuries: posterior cruciate ligament tears

Introduction
The posterior cruciate ligament (PCL) is the strongest intraarticular ligament of the knee and a primary joint stabilizer(1). Three percent of knee injuries at outpatient departments and 38% of acute knee hemarthroses involve the PCL(1). Isolated PCL tears are rare, and in 95% of cases, PCL tears coincide with other ligament tears(1). Posterior cruciate ligament injuries are considerably less common than anterior cruciate ligament (ACL) injuries; therefore, the long-term management of isolated PCL injuries is under-researched(2).Anatomy and Biomechanics
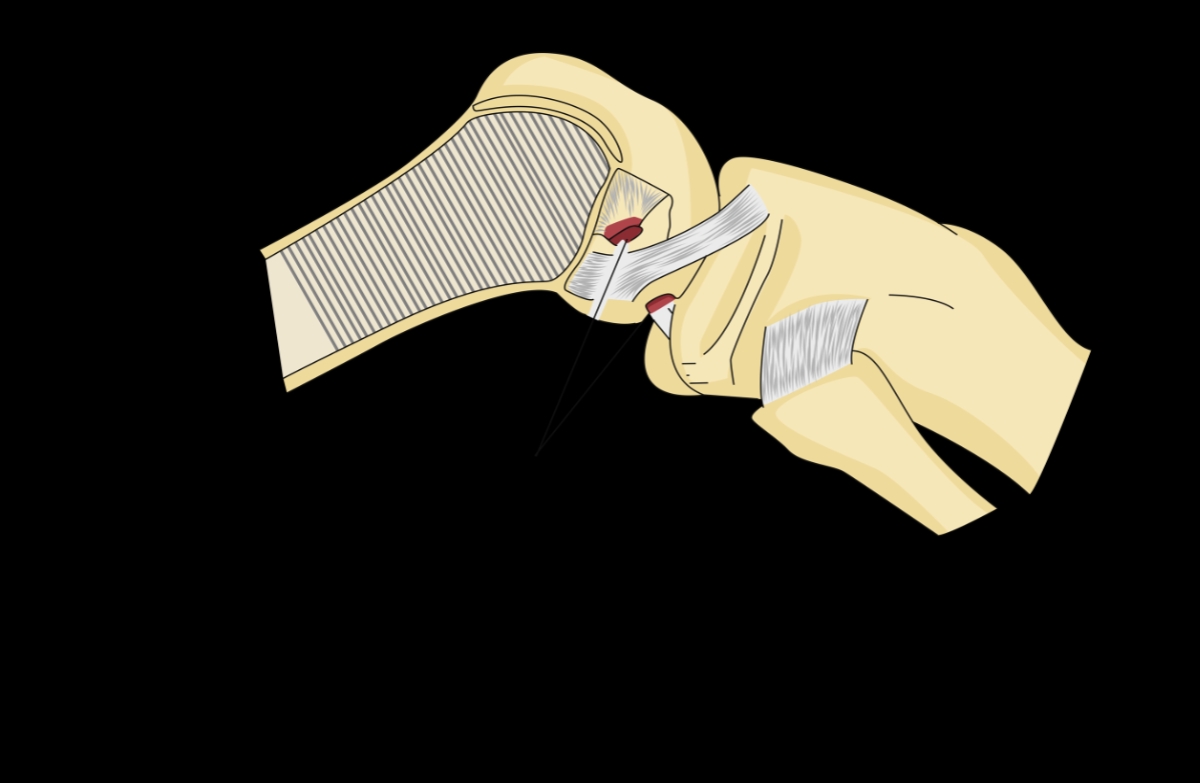
The PCL has two functional bundles. The anterolateral bundle (ALB) and the other being the posteromedial bundle (PMB)(1). The PCL, alongside the ACL, is extra-synovial, although it resides within the joint capsule. A synovial sheath covers both the PCL and ACL and shields them from the synovial fluid(3). The PCL originates from the anterolateral aspect of the medial femoral condyle within the intercondylar notch and inserts on the posterior aspect of the tibial plateau (see figure 1)(3). The length of the PCL ranges from 32-38mm, and it is almost twice as thick as the ACL(3). Branches of the tibial nerve innervate the PCL, and its blood supply comes from the middle geniculate artery(3). Two different meniscofemoral ligaments reinforce the integrity of the PMB, the anterior meniscofemoral ligament, known as the ligament of Humphreys, and the posterior meniscofemoral ligament, called the ligament of Wrisberg.Figure 1: The origins of the PCL and the ACL

The PCL prevents posterior movement of the tibia on the femur at all knee flexion angles(3). The PMB prevents internal rotation of the knee between 90º and120º of knee flexion(1,3). During knee flexion, the PMB is lax, and the ALB is tight. Conversely, the PMB is tight in knee extension, with the ALB being lax(3). The two bundles work together to resist tibial translation posteriorly. A complete rupture means both bundles are torn(1). A PCL deficient knee exhibits excessive rotational movement beyond 90º of knee flexion(3). In addition, maximal posterior tibial translation on the femur occurs at 90º degrees of knee flexion compared with the contralateral healthy knee(4,5). The PCL can sustain tensile forces of up to 739N to 1627N, with most of the force absorbed by the ALB(3). The ALB is twice as big as the PMB and is the primary stabilizer felt during a posterior draw test(4,5).
Mechanism of injury
The PCL is typically injured when a car dashboard applies a posteriorly-directed force on the tibia while the knee flexes (see figure 2)(6). This same posteriorly directed force can occur during high-energy sporting activities. For example, a goalkeeper who collides with an attacking player while in a flexed knee position may experience a similar force. When this action is coupled with rotational or coronal plane forces, the medial and lateral collateral ligaments are also at risk for injury.Figure 2: Mechanism of injury. A posterior force on the tibia can strain or tear the PCL.
Clinical Tests
There are 11 clinical tests for PCL instability (see table 1)(7). A systematic review assessed the 11 tests across 11 studies and found the results inconclusive as to which test was most accurate. However, compared with other tests, the posterior drawer test has a sensitivity of 90% and a higher specificity of 99%(8). Perform the posterior drawer test (see figure 3) with the patient supine and the knee flexed to 90º(5). Start with the anterior border of the lateral tibial plateau positioned 1cm anteriorly to the lateral femoral condyle. Without this reference point the examiner may obtain a false negative for a posterior drawer test and a false negative for an anterior drawer leading to an incorrect diagnosis(5).| Clinical Test |
|---|
| Posterior Drawer Test |
| Quadriceps Active Test |
| Recurvatum Test |
| Posterior Sag Sign |
| Valgus/Varus at 0° |
| Reverse Lachman Test |
| Dynamic Posterior Shift |
| Reverse Pivot Shift |
| Reverse Lachman End Point |
| Valgus at 30° |
| Varus at 30° |
Figure 3. The posterior Drawer Sign.

Long Term Management of PCL Injuries
Traditionally, clinicians choose conservative management for patients with isolated PCL tears that exhibit less than 10mm posterior translation or less than 5° rotational laxity(2,9). The possible long-term effect of a PCL deficient knee is chronic pain, discomfort during activity, joint effusion, articular cartilage degeneration, and functional instability(2). An isolated PCL rupture can have degenerative effects on the meniscus in young athletic individuals(10).Research from the national defense medical center in Taiwan studied the effects of a PCL tear with or without reconstruction over 15 years(2). The study included 4,167 patients diagnosed with PCL tears and assessed for meniscal tears, osteoarthritis (OA), and total knee replacement (TKR). In comparison, the study included 16,676 without PCL injury as a control cohort with a mean age of 32.54 years across the two studies.
There was a significant effect (P<0.001) observed between the groups for meniscal tears with 1.13% in the PCL group (n=47) compared to 0.22% (n=37) in the control group. Posterior collateral ligament tears also significantly influenced (P<0.001) the onset of OA, with 2.71% (n=113) in the PCL group and 1.9% (n=317) in the control group showing signs of joint deterioration. A further significant effect (P<0.041) was noted in those having TKR with 0.91% (n=38) in the PCL group and 0.62% (103) in the control group. The results of this long-term cohort study show that PCL insufficiency has detrimental effects on the knee joint.
Non-operative Treatment
Consider a nonsurgical approach for a PCL tear that is a Grade I or II in an athlete or a Grade III in a person with a low activity level (see table 2)(6). Other factors that warrant consideration when deciding the best management approach are the posterior tibial slope, inherent knee laxity, and quadriceps strength(6). A UK study investigated the effects of non-operative management of isolated PCL injuries in 46 athletes with a grade II (n=25) or a grade III (n=21) tear(11). Rehabilitation began four weeks after the injury in those included in the study, with a mean return to training at 10.6 weeks and a mean return to competitive sport at 16.4 weeks post-injury. At the five-year reassessment, 32 (69.5%) subjects played at the same level as pre-injury, and 38 (82.6%) were still playing at a competitive level.| Protective, Phase 1 “ weeks 1 - 6 | Depending on the degree of instability, immobilize the knee for 2 to 4 weeks. Use a PCL-specific brace that is going to apply correct joint forces and resist posterior translation. This aids healing and prevents elongation of a still intact ligament. The brace may be limited to 90º degrees knee flexion for the first two weeks. |
| Regain quadriceps activity to achieve a straight leg raise without knee lag. | |
| Once the brace is off, begin proprioception exercises in a two-legged stance with a progression onto a wobble board and progress to a single-leg stance. | |
| Knee flexion in a loading position is limited to 70 degrees to control the load on the healing PCL. | |
| Transitional, Phase 2 “ weeks 6 - 12 | Increase proprioception and strengthen the lower limb using closed kinetic chain exercises such as double leg squats and leg presses. Avoid shifting away from the painful side. |
| All activities should be pain-free and without causing effusion. Achieve and maintain full range of motion. | |
| Aim to avoid knee hyperextension to prevent excessive load on the PCL. | |
| Increase the challenge during proprioceptive exercises to include single-leg drills and unstable surfaces. | |
| Functional, Phase 3 “ weeks 12-16 | Closed kinetic chain exercises should advance beyond 70º knee flexion. Perform isolated hamstring exercises as tolerated. Core stability, neuromuscular control, and proprioception-based exercises should be done under control and begin running once theres adequate single-leg stability and strength. |
| Commence agility work while managing load and monitoring for quality of movement. | |
| Return to play, Phase 4 “ weeks 16 - 24 | Include sports-specific agility and dynamic stabilization drills and monitor for compensatory movements that may lead to re-injury. |
| Continue to improve strength in the involved leg with a focus on single-leg stability. |
Conclusion
Because they are rarer, PCL injuries are less well understood than ACL tears. The research is improving, particularly with regards to the long-term effects of a PCL deficient knee. Conservative management with an effective rehabilitation program allows some athletes to return to sport.References
- Arch Bone Jt Surg. 2018;6(1):8-18.
- PLoS ONE. 2018 Oct;13(10):e0205118.
- Curr Rev Musculoskelet Med. 2018 Sep;11(3):510–14.
- Am J Sports Med. 2013 Dec;41(12):2828-38.doi: 10.1177/0363546513504287
- documentcloud.adobe.com/link/review?uri=urn:aaid:scds:US:7db92733-3bdb-4f55-b0a5-c50d493e73d6
- Curr Rev Musculoskelet Med. 2018 June;11(2):290-297.
- 2013 Nov;43(11):804 – 816.
- The Am J of Sports Med. 1994;22(4):550-557.
- The Am J of Sports Med. 2004 Oct;32(7):1765-1775.
- Knee Surg Sports Traumatol Arthrosc.2015 Oct;23:3094–3100 (2015).
- Bone Joint J2017;99-B(6):774–8.
Related Files
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










