You are viewing 1 of your 1 free articles
Tibialis anterior herniation in the athlete: a fascial defect condition?

Muscle herniation, also known as a myofascial defect, is the protrusion of a muscle through the surrounding fascia. The most common location of muscle herniation is in the leg. Because this injury is tricky to diagnose and rarely reported, there is little data in the literature upon which to draw(1-3). A surge of reports of lower-extremity muscle hernias in physically active military recruits appeared in military medical journals during the 1940s(4-7). Therefore, the majority of early research on leg hernias (and much of our current knowledge) stems from the efforts of military surgeons.
Tibialis anterior hernia incidence
The true incidence of leg hernias is not known. Many are asymptomatic and, thus, remain undiagnosed(8). The most commonly diagnosed muscle herniation is of the tibialis anterior (TA)(9-12). Herniation at this location is likely because the fascia of the tibialis anterior is weak and vulnerable to trauma(13). Though less common, other lower-limb muscles can herniate, including the peroneus brevis(14), extensor digitorum longus(15), gastrocnemius,(16) and flexor digitorum longus (see figure 1)(6).Figure 1: Cross-section of lower limb showing fascial compartments

TA = tibialis anterior; TP = tibialis posterior; EHL = extensor hallucis longus; EDL = extensor digitorum longus; FDL = flexor digitorum longus; FHL = flexus hallucis longus; PB = peroneus brevis; PL = peroneus longus
Etiology of tibialis anterior hernia
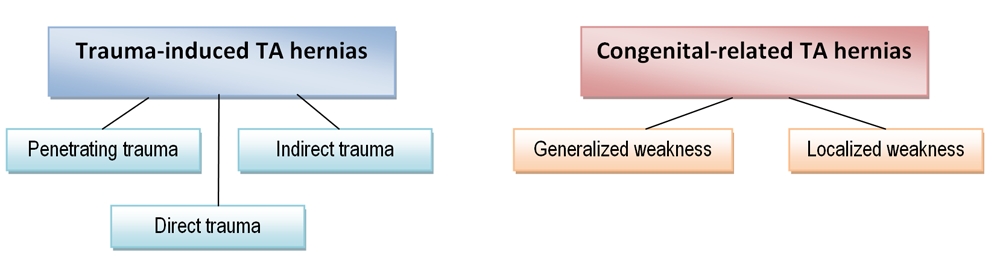
Tibialis anterior hernias are typically associated with trauma, direct or indirect, and congenital weaknesses of the fascial tissue surrounding the TA (see figure 2). Traumatic examples include(17):- Penetrating trauma
- Closed fracture that causes a fascial tear (direct trauma)
- Force applied to the contracted muscle causing acute fascial rupture (indirect trauma)
Congenital weakness may involve the fascial tissue as a whole or only a localized site where blood vessels and nerves pass through the fascia(18).
Athletes who suffer a TA hernia without a history of trauma are likely to have some degree of congenital weakness in the TA fascial tissue. Studies suggest that fascial defects are more common than appreciated. For example, one study found that fascial defects were present in 15% to 50% of patients undergoing surgery for chronic exertional compartment syndrome (CECS) – even though pre-operation examinations were normal(19). Because increased intracompartmental pressure potentiates herniation, soldiers, athletes, mountain climbers, skiers, etc, are at much greater risk of developing a TA hernia than the population at large(20,21).
Figure 2: Overview of TA hernia etiology
Signs and symptoms
A patient with a TA hernia typically presents with a range of symptoms, including:- A localized swelling or nodule(s) over a portion of the anterior shin, which is soft and may be mildly tender.
- A dull pain localized to the site of the swelling that increases upon weight-bearing and activity.
- Cramping, discomfort, weakness, or neuropathy.
- Possible numbness in the lateral portion of the lower leg and foot of the affected side.
- A decrease in swelling when in the supine position. This reduction may also occur with muscle inactivation.
- An increase in localized pain and swelling size when the lower leg is placed in the ‘fencer’s lunge’ position (see figure 3).
The differential diagnoses of these symptoms should include the following which present similarly(18):
- Lipoma
- Hematoma
- Fibroma
- Epidermoid cyst
- Tumor
- Angioma
- Arteriovenous aneurysm
- Ruptured muscle
- Central neuropathy
A correct diagnosis of TA herniation enables the athlete to start rehab immediately, and prevents unnecessary diagnostic procedures and associated psychological stress.
Although the data is limited, it is common for patients to display normal strength and patellar/Achilles reflexes. In TA cases of traumatic origin, patients may report having experienced particularly intense pain at the time of injury, and there may be a sign of the original trauma. In congenital cases, no signs of trauma will be evident. If the observed swelling/nodule is palpable and reducible with muscle inactivation or the adoption of a supine position, clinicians can feel fairly confident that a hernia is present. Therefore, without clinical and orthopedic red flags, there’s typically no need for further diagnostic procedures, especially following trauma(22). Magnetic resonance imaging (MRI) and ultrasound imaging can help confirm the diagnosis.
Figure 3: Fencer’s lunge position

Imaging
Although MRI allows better visualization of the muscle-fascia demarcation, and determination of herniated muscle volume, the gold standard for imaging, is ultrasonography due to its relative ease and low cost(23). If available, 3-dimensional dynamic ultrasound scanning with surface rendering is superior to traditional two-dimensional scans since it provides better visualization of the fascial planes and muscular protrusion(24). However, magnetic resonance imaging comes into its own should conservative treatments for a TA hernia fail and surgery is needed, or when ultrasound imaging is inconclusive. In particular, it assists in surgical planning by assessing neighboring neuro and musculoskeletal tissues, quantifying fascial splitting, and determining the degree of muscle herniation.Treatment options
There’s no clear consensus on conservative treatment protocols for TA herniation. In the case of an asymptomatic TA hernia (which the clinician is less likely to encounter), patient reassurance and education are all that is required(25). However, when painful symptoms are present, manage conservatively with rest, load modification, and compression stockings(26).Some research suggests that a more proactive approach, combining isometric, eccentric, and plyometric exercises, yields useful results(27). In this case study, the patient – a 28-year-old male soccer player presenting with a trauma-induced TA herniation injury to his right anterior shin undertook the following protocol:
- Stage 1 (approx. two weeks) – Rest (i.e., non-weight bearing), the use of compression stockings, and isometric contraction exercises for the tibialis anterior muscle (in the supine position to minimize any potential intracompartmental pressure from weight-bearing). The use of isometric contraction helps activate high-threshold motor units involved in exercise-induced analgesia(28).
- Stage 2 (approx. two weeks) – Exercise loading progressed to concentric contraction of TA muscle in supine and in weight-bearing positions.
- Stage 3 - Eccentric exercises were employed for the TA muscle to generate force over a greater muscle length and stimulate maximal tissue adaptation to elastic force. This mode of exercise appears effective because the elastic energy stored during the lengthening phase of the eccentric contraction can be used during the shortening phase of muscular contraction to amplify force and power production during exercise(29).
- Stage 4 - In the last stage of rehab, sports-specific plyometrics exercises were introduced to generate sports-specific multidirectional force and stability through neural adaptation.
Surgical treatment
When TA herniation occurs as a result of trauma, a graded, stepwise, conservative treatment approach may produce good results within eight weeks. However, where the cause is congenital, or there is a history of chronic TA herniation, surgical repair may be needed. Traditionally, the most commonly used surgical technique is the direct closure of the fascia defect by tightening the area. However, a retrospective analysis of this procedure concluded that this often results in a high re-herniation rate and increases intracompartmental pressure, which predisposes the patient to compartment syndrome later(30). A more successful and current surgical approach is a longitudinal decompressive fasciotomy, which results in less intracompartmental pressure and lower rate of re-herniation. An alternative surgical option is to repair the fascia using synthetic patches.References
- Br J Plast Surg. 1976;29:291–4
- 1943;1:602–3
- Am J Surg. 1945;67:87–97
- Br J Surg. 1949;36:405–8
- Bull US Army Med Dept. 1944;77:111–2
- US Naval Med Bull. 1943;41:404–9
- Mil Surg. 1943;93:308–10
- J Am Med Assoc. 1951 Feb 24; 145(8):548-9
- Skeletal Radiol. 1999;28:465–9
- Clin Orthop Relat Res. 1989:249–53
- Dermatol Surg. 2002;28:641–2 2012;2:42–4
- J Am Acad Dermatol. 1990;22:123–4
- Br J Dermatol. 1976;95:329–30
- J Bone Joint Surg Am. 1977 Apr; 59(3):404-5
- PM R. 2009 Dec; 1(12):1109-11
- 2010 Nov; 33(11):785
- Orthop Rev. 1993 Nov; 22(11):1246-8
- Can J Plast Surg. 2013 Winter; 21(4): 243–247
- Clin Orthop Relat Res. 1987;220:217–27
- Int J Sports Phys Ther. 2011 Jun; 6(2):126-41
- Azar FM. Sports Medicine. In: Canale ST, Beaty JH, editors. Campbell’s Operative Orthopaedics. 12th edn. Vol. 3. Philadelphia: Mosby/Elsevier; 2012
- Clin Orthop Rel Res. 1989; 244: 249
- Crit Ultrasound J. 2014; 6(14)
- J Ultrasound Med. 2007 Feb; 26(2):239-42
- Muscle Ligament Tendon J. 2015;5(4): 331-334
- Am J Clin Dermatol. 2012;13:293-310
- J Can Chiropr Assoc. 2020 Apr;64(1):88-91
- Med Sci Sports Exerc. 2008;40(11): 1880-1889
- J Orthopedic Sport Phys Ther. 2003;33: 557-571
- J Bone Joint Surg. 1986;68: 1444-1445
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.






