You are viewing 1 of your 1 free articles
Running injuries: the art and science of prediction

Running is beneficial for general health, and while some runners train to compete in race situations, more runners are recreational who run mainly for fitness and fun. These runners often complete just a few kilometers per training session(1). However, despite the extensive health benefits that running brings, the risk of lower-limb injury is comparatively high. For example, in a 6-month study of 87 recreational runners, 79% suffered at least one lower-limb injury during the observation period(2). Another study observed 583 habitual recreational runners over 12 months. In this cohort, 252 men (52%) and 48 women (49%) reported at least one lower-limb injury severe enough to affect running habits, require a visit to a health professional, or necessitate the use of medication(3). Among the wider running population, the risk of sustaining a lower-limb injury ranges between one injury per 147 hours of training and 17 hours of training(1).
Identifying risk
Known risk factors for injury among non-elite runners include(1,4):- A previous running-related injury.
- Running more than 64kms per week.
- Speed work and interval training.
However, identifying these kinds of associations is a rather blunt tool for clinicians. Runners with similar training histories and protocols don’t experience the same injuries at the same time. These associations tell you what factors might increase the overall risk but not which runners are more at risk.
Several studies have taken a more analytical approach by comparing biomechanical attributes in injured and non-injured runners. These include:
- External knee adduction moments(5).
- Ankle eversion range of motion and eversion velocity(6).
- Hip musculature strength(7).
Studies that compare biomechanical aspects of movement in a cohort of injured subjects with those from a different group of non-injured runners are less than ideal. One reason is that many of these studies provide the relative risk of injury data instead of the actual risk. For example, a study at Wake Forest University examined the effect of knee stiffness on injury rates. The researchers compared injured and non-injured runners and found that those with a high level of knee stiffness were 18% more likely to suffer an injury than those with low knee stiffness(8). However, while informative, it gives little idea of actual risk in a runner. If the risk of a knee-stiffness related injury is only one injury per 5,000 hours of running, an 18% increase is still a minuscule risk overall. However, if it is as high as one in 20 hours, it’s a risk that is well worth addressing.
A better approach is to take injury occurrence in the same cohort of runners performing the same training over an extended period and identify the biomechanical factors that are associated with an injury. This method allows an absolute measure of risk and enables clinicians to determine who is most susceptible to getting hurt. By providing suitable training interventions to help mitigate these factors, therapists can help reduce the risk of injury going forward.
Cohort study
Although few studies use the cohort approach, a study published by Swedish scientists provides valuable insight(9). Researchers recruited 224 runners from the Gothenburg Half Marathon e-mail lists and tracked them for one year. Runners were:- Between 18 and 55 years-old.
- Without musculoskeletal injuries in the lower extremities six months prior to the pre-study baseline examination.
- Running at least 15kms per week (on average) for the 12 months before the baseline examination.
- Running without orthopedic insoles.
- Not pregnant.
- Not diabetic.
The baseline clinical/anthropometrical examination consisted of the following:
- An assessment of joint range of motion, muscle flexibility, and trigger points.
- A biomechanical running analysis, which assessed lower limb running kinematics.
- Isometric strength tests.
Following the baseline examination, the investigators instructed the runners to maintain their regular training and report training characteristics and pain weekly. At the end of the 52-week monitoring period, the incidence of running-related injuries (RRIs) – as diagnosed by a medical practitioner – was recorded. To ensure consistency, researchers defined RRIs as:
“A running-related musculoskeletal pain in the lower limbs or back that causes a restriction on or cessation of running (distance, speed, duration or training) in more than 66% of all training sessions over two consecutive weeks, or in more than 50% of all training sessions over four consecutive weeks, or that requires the runner to consult a physician or other health professional(9).”
The findings
Over one year, the runners averaged 25kms per week and sustained a total of 85 injuries. The data found no associations between an RRI and excessive or restricted joint range of motion, extreme or limited muscle flexibility, or painful trigger points. There were, however, two factors that were significantly associated with sustaining an RRI:- Kinematics: late timing of maximal eversion – correlated with 55 injuries in the cohort (see figure 1)(9).
- Strength: weak hip abductors in relation to hip adductors – correlated with 57 injuries(9).
Figure 1: Ankle eversion (vs. inversion)
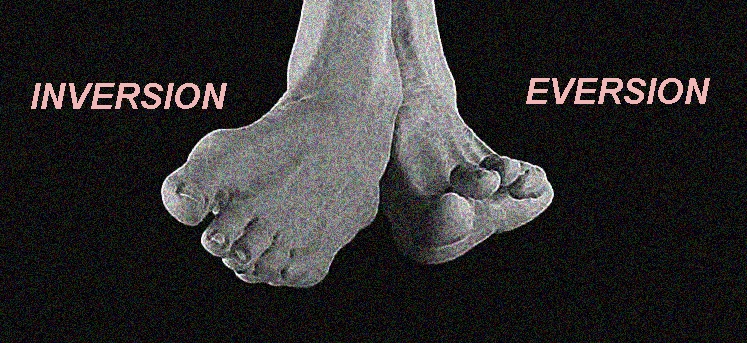
The association between late ankle eversion and an RRI might indicate insufficient neuromuscular activation of the tibialis posterior (see figure 2), since this muscle works eccentrically during the pronation phase of running gait(9). While other researchers suggest this variation is not always predictive of RRIs, it’s prudent for clinicians to pay attention to runners with late ankle eversion(10). When observed, the addition of exercises targeting and activating the tibialis posterior may prove beneficial.
The double-leg heel raise while squeezing a tennis ball is an excellent and simple exercise to increase tibialis posterior activation (see figure 3). Pay particular attention to the lowering (eccentric) phase of the exercise in order to maximally activate fiber movement patterns used during the pronation phase of running.
Figure2: Anatomy of tibialis posterior

View from behind the lower leg showing the full length of the muscle, with the tendon located medially behind the medial malleolus.
Figure 3: Double-leg heel raise
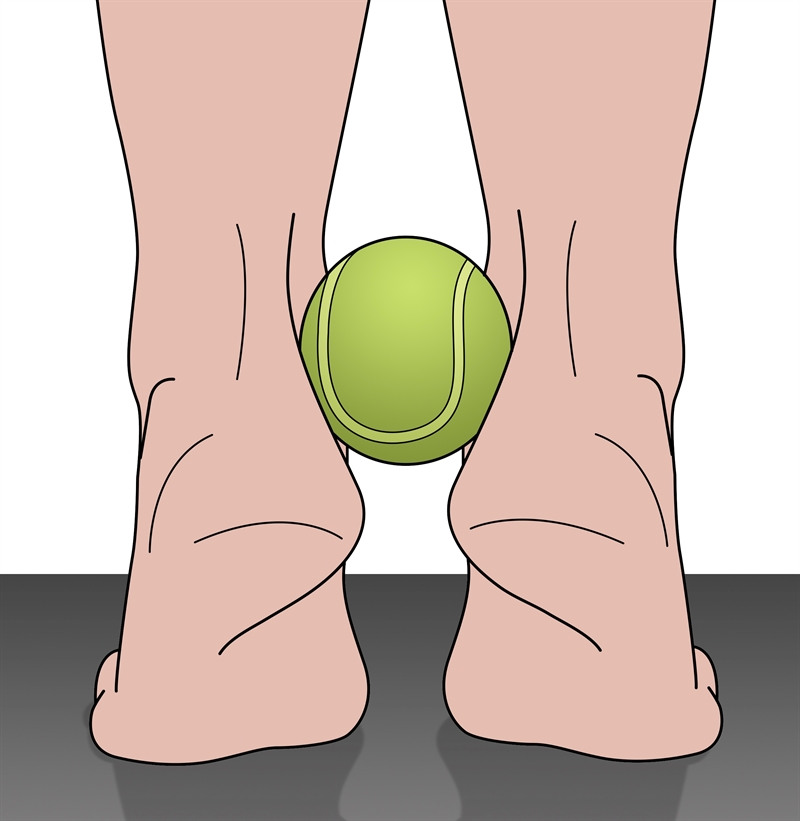
Perform this exercise while squeezing a tennis ball to encourage correction of rearfoot eversion. Emphasize the eccentric phase of lower heels.
Hip abductor strengthening
Reduced hip abductor strength was significantly associated with an increased risk of RRI in the Swedish study, and is a common finding among injured runners(11). To address this weakness, prescribe functional exercises that develop the dynamic hip control needed in running. These activities integrate dynamic abductor and external rotation muscle control using functional movements such as a short hop and stop.Here is one variant:
- Place a broomstick or light barbell on the athlete’s shoulder and have them stand on one leg (the stronger leg) in front of a mirror.
- The broomstick reflects the action of the pelvis. If one side of the broomstick drops as the athlete hops onto the other foot, it indicates an inability to maintain a neutral pelvis. This reproduces the same action as foot strike in running.
- While this is a test, it is also a motor control exercise, which requires repeat efforts (with rest periods) to ensure that every repetition is done perfectly.
- Once motor control can be maintained, it is then possible to load this exercise with a weight placed on the barbell opposite the side that needs training.
Figures 4 and 5: The start and finish position of the short hop and stop hip abductor strengthening exercise

The aim of this exercise is to train the dynamic control of the left hip.
In summary
The risk of sustaining an RRI in recreational runners running modest distances over a year is around 38%. The biomechanical factors that significantly correlate with an RRI are late timing of ankle eversion (most likely as a result of reduced tibialis posterior activation) and hip abductor weakness relative to adductor strength. Given that conditioning exercises can help to remedy these biomechanical traits, clinicians may find kinematic and strength screening beneficial for runners in their care.References
- J Physiotherapy 2013; 59(4) 263-269
- Br J Sports Med . 2004 Oct;38(5):576-80
- Arch Intern Med. 1989 149(11):2565-8
- Archives of Internal Medicine, 149 (1989), pp. 2565-2568
- Hum Mov Sci. 2017;52:197
- Hum Mov Sci 2016; 47 9-15
- PM&R 2011; 3 (9)792-801
- Am J Sports Med . 2018 Jul;46(9):2211-2221
- Inj Epidemiol. 2020; 7: 10. doi: 10.1186/s40621-020-00237-2
- Sports Med. 2019. 10.1007/s40279-019-01110-z
- J Orthop Sports Phys Ther 2010;40(2):42–51
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










