You are viewing 1 of your 1 free articles
Posterior shoulder laxity: more common than we thought?

Posterior instability is a relatively uncommon condition, typically reported in athletes who participate in contact or overhead sports. It is reported to represent as little as 10% of all shoulder instability cases(1,2). It can occur as a result of either acute trauma or repetitive micro trauma, and is commonly seen in athletes with multidirectional instability(1).
Posterior instability can be hard to diagnose clinically, and it often coexists with other shoulder pathologies. However, with increasing awareness of this condition, the incidence of posterior instability - particularly in the overhead athlete - is likely to be more common than previously thought.
Anatomy
The glenohumeral joint is the most mobile joint in the body. This mobility is integral to the performance of the overhead athlete but it often comes at the expense of stability. At any given time only about one third of the humeral head is articulating with the glenoid fossa(1). The glenoid labrum provides some passive stability by attaching onto the periphery of the glenoid fossa, and it effectively deepens the glenoid socket(1). The postero-inferior capsule and inferior glenohumeral ligament are the primary restraints to posterior instability at 90 degrees of abduction(1). Any injury to these structures, or abnormalities of bony morphology (glenoid hypoplasia, excessive humeral or glenoid retroversion or posterior glenoid erosion), can predispose an athlete to posterior instability(3).As well as the passive stabilisers in the shoulder (the rotator cuff muscles), the long head of biceps and the deltoid also provide dynamic stabilization of the shoulder. Contraction of these muscles compresses the head of the humerus into the glenoid and as a consequence, they become particularly important to stabilise the shoulder if there is any disruption of the passive stabilising structures(1).
Pathology and classification
Classification of posterior instability remains controversial and currently, no standardised system has been agreed upon or is routinely used. The mechanism of injury, severity, direction of instability, presence of ligamentous laxity and presence of volitional instability have all been considered when classifying glenohumeral instability.Posterior instability can be described as either ‘traumatic’, ‘repetitive overuse’ or ‘due to soft tissue disorders’(2). Acute traumatic posterior shoulder dislocation is 15-20 times less common than anterior dislocation(2). The most commonly described mechanisms of frank posterior dislocations are as follows:
- Acute trauma- ie landing on hand/elbow with arm in flexed/horizontally adducted and internally rotated position and/or car accident with hand on steering wheel.
- Electric shock
- Seizure
(NB - Seizures and shock can cause shoulder dislocations because they produce extreme, unbalanced muscle contractions that can wrench the humerus out of place).
Athletes who experience a posterior shoulder dislocation may present with detachment of the posterior labrum from the glenoid rim (a ‘reverse Bankart lesion’ – see figure 1). When the labral detachment is associated with a piece of the glenoid rim being avulsed, this is referred to as a ‘reverse bony Bankart lesion’(1).
Figure 1: Reverse Bankart lesion
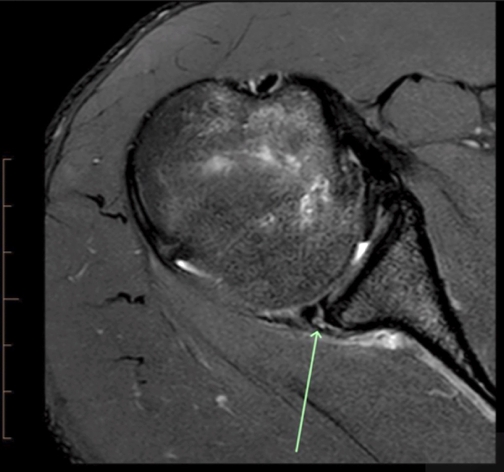
Location of lesion arrowed
Structural lesions associated with posterior instability may include:
- Inferior glenohumeral ligament injury.
- Reverse Bankart lesion.
- Reverse Hills-Sachs lesion.
- Reverse humeral avulsion of the glenohumeral ligament (HAGL).
- Posterior labral tears.
- Kim lesion (tear between the posterior labrum and glenoid cartilage without detachment).
The clinician should also be aware that a locked dislocation can occur; in this instance, the patient would have altered contour (flattened) of the joint anteriorly(3).
The predictors of recurrent instability in the acute setting are:
- An age of less than 40years.
- A large reverse Hills-Sachs lesion.
- Seizure as the initial cause.
More commonly in the overhead athlete, posterior instability occurs due to either generalised hypermobility or repetitive microtrauma. It is hypothesised that in positions of flexion, adduction and internal rotation (ie follow through throwing or backhand in tennis), the posterior structures of the shoulder will become stretched over time. Without adequate dynamic control in these positions, the posterior structures of the shoulder stretch, resulting in laxity and eventually instability.
Clinical examination
*Subjective
The overhead athlete with posterior instability often reports vague symptoms - either anterior or posterior shoulder pain - which in most cases does not describe a dislocation or instability. They may describe weakness, a feeling of fatigue or they may have mechanical symptoms such as clicking or locking(1). They will typically describe pain in their shoulder during activities that involve a combination of flexion, horizontal flexion and internal rotation(2). This includes activities such as throwing, turning a steering wheel, bench press or overhead weights.
To determine whether the injury is due to acute trauma or repetitive overuse, initial questioning should focus on whether there has been a single traumatic event, as a specific incident may be indicative of structural lesion of significance(2). Commonly, a feeling of instability is a secondary concern - particularly in the hypermobile population - as they may not be aware that their humerus has developed increased translation because they have always ‘clicked’ or ‘clunked’(2).
*Objective
As with all shoulder injuries, a thorough assessment of both shoulders should be conducted including scapula position, shoulder ROM, strength and palpation. Cervical spine assessment should also be conducted to determine if any cervical spine involvement is present.If posterior instability is suspected than specific tests for the posterior shoulder should be conducted. These include the posterior drawer, jerk, and Kim tests (see figures 2, 3, and 4).
Figure 2: Posterior drawer

This test can be conducted in either supine or sitting. The examiner stabilises the glenoid with one hand whilst the other hand applies a posteromedial directed onto the humerus. The examiner assesses for any excessive posterior translation. This can be graded as:
Grade 1- less than glenoid margin.
Grade 2- beyond glenoid margin/reduces.
Grade 3- beyond glenoid margin/does not spontaneously reduce.
Figure 3: Jerk test

The patient sits with their arm in forward flexion, adduction and internal rotation. The examiner applies a posterior directed force along the line of the humerus, which causes posterior translation of the humeral head. A positive test demonstrates a clunk (+/- pain) as the patient’s arm is then horizontally extended back to neutral. A positive clunk may be indicative of a posterior labral tear(1).
Figure 4: Kim test

The patient sits with the shoulder abducted and internally rotated. The examiner holds the patient’s bicep with one hand and their elbow with the other. Whilst the arm is elevated to 135 degrees, the examiner applies an axial load to the elbow causing it to posteriorly translate out of the socket. A positive test is represented by pain, clunk or a click(1).
As posterior instability is often present in multidirectional instability, all patients with suspected posterior instability should also be tested for anterior and inferior instability. Common tests for these pathologies are outlined below:
Anterior instability
- Apprehension
- Load and shift
- Apprehension/relocation tests
Inferior Instability
- Sulcus test
General hypermobility should also be tested using the Beighton score and an overall score greater than 4 would indicate generalised hypermobility syndrome (see table 1).
| Test | Score - Test L and R side where applicable; Score 1 point for each side that tests positively. |
|---|---|
| Hyperextension elbow > 10deg | x/2 |
| Hyperextension of knee > 10deg | x/2 |
| Passive extension of little finger > 90deg | x/2 |
| Passive apposition of thumb to flexor aspect of forearm | x/2 |
| Forward flexion of trunk with knees straight and palms flat on floor | x/1 |
As well as these specific tests, the clinician should also try to determine whether scapula or head of humerus repositioning will be the main component of the athlete’s rehabilitation plan. To do this, the clinician firstly observes a provocative movement and determines whether an abnormal movement pattern is present. The clinician then gets the patient to repeat the provocative movement whilst the clinician corrects an abnormal movement pattern (either scapula or head of humerus repositioning – see figures 5 and 6). If there is improvement in the patient’s symptoms, ROM or strength then this gives the clinician the ‘treatment direction’, and highlights to both the patient and the clinician that treatment directed at correcting the abnormal movement is likely to be successful.
Figure 5

Shows head of humerus correction, supporting posterior aspect of the shoulder whilst the patient performs shoulder flexion.
Figure 6

Shows correction for the common depressed and downward rotated scapula. If a correction makes the symptoms worse then consideration must be given to the fact the abnormal movement may be an adaptive response to injury/instability to help stabilise the joint.
Treatment
In most cases conservative treatment should be the first line of treatment for posterior instability. Patients with a traumatic history are more likely to have structural lesions, and as a result tend to have less favourable outcomes with conservative treatment than those with non-traumatic instability(3). The initial focus of rehabilitation is directed by which correction technique (scapula or head of humeral correction) was most successful in alleviating the patient’s symptoms.Scapula correction drills
If scapula correction alleviated the patient’s symptoms then the initial phase of treatment should focus on improvement of the scapula position. The aim of this phase is to develop adequate scapula control and centering of the head of humerus, so the shoulder has a stable base to work from.
Initially scapula correction drills should be started in either side lying, or sitting or standing with the arm by the side (see figure 7). Commonly, the scapula is anteriorly tilted/downwardly rotated, protracted and depressed (or a combination of those).
Figure 7: Scapula control exercise

Scapula control exercise using theraband to help elevate, retract and posteriorly tilt the scapula.
Head of humerus correction drills
These drills can be broken down into four phases and should be commenced either when sufficient scapula control is achieved, or if head of humerus repositioning was the most successful way of relieving the athlete’s symptoms. The main aims are to improve activation and strength of the scapula stabilisers, posterior rotator cuff and posterior deltoid, as these all help to control posterior translation of the head of humerus. Scapula control should continue to be emphasised during this phase and shoulder ROM should be progressed, initially commencing with movements that do not place posterior translation forces on the head of humerus.
Phase I
These include shoulder extension (to neutral), external rotation, horizontal extension (see figure 8). During this early phase, particular care should taken to avoid positions that either traction the gleohumeral joint or have a posterior translation force on the humerus (ie weight bearing through the arm in positions of shoulder flexion).
Figure 8: Phase 1 exercise example

Phase II
This phase aims to improve head of humerus control in positions up to 90 degrees in both the sagittal and coronal plane. The athlete initially commences with exercises at lower ranges of abduction and then into flexion. Once these have been achieved with satisfactory strength, higher ranges of abduction and flexion can be introduced. These exercises are designed to increase recruitment of posterior deltoid and the posterior cuff to help control posterior translation of the humeral head (see figures 9a and 9b).
Figures 9a and 9b

a) Scapula setting with ER on 90 degrees abduction

b) Resisted horizontal extension on 90 degrees abduction
Phase III
This phase includes exercises above 90 degrees that replicate the demands of the sport, and also progressing to drills in ranges of horizontal flexion (see figures 10a and b).
Figures 10a and 10b

a) Top of ‘lawnmower exercise’ using uninjured side to assist

b) Eccentric phase of ‘lawnmower exercise’ lowering back to start position
Phase IV
Once the athlete has completed stage III, he/she can commence a sport-specific return. In the case of a throwing athlete, this would mean a graduated return to throwing, starting at low intensity over shorter distance then gradually increasing distance and then intensity. An athlete who has an episode of posterior instability should remain on a maintenance program even once they have returned to sport - to ensure good activation and strength is maintained.
Conclusion
The incidence of posterior instability is likely to be more prevalent than currently reported particularly in the overhead athlete. With increasing awareness of this condition and appropriate testing, the astute clinician will be able to correctly identify those athletes with posterior instability, and an appropriate and progressive rehabilitation program can then be implemented.References
- Sports Medicine Arthroscopy Review 2017. Vol 25 , No 3, 136-143
- Clinical Sports Medicine 2013. Vol 32 685-696
- Journal of Hand Therapy 2017. Vol 30 182-192
- Journal of Arthroscopic and related surgery 2011. Vol 27 p1562-1572
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









