You are viewing 1 of your 1 free articles
Lumbar transverse process fracture in sport: rare or underreported?

Most of the reported transverse process fractures (TPFs) result from high-impact traumas, such as traffic accidents(1-4). The high-energy traumas that cause TPF fractures usually also result in complex underlying injuries(5). However, in athletes, TPFs happen in isolation, likely because of a much lower-energy mechanism of injury(6). Because of these differences, definitive diagnosis and injury management strategies gleaned from the general population may not apply to athletes
TPF injury in sport: how common?
Transverse process fractures caused by stress are likely under detected since even an acute transverse process fracture requires a high index of suspicion to be correctly identified(4,7). However, since TPFs can also occur due to repetitive loading, this underreporting may be quite significant(8).Given the lack of research on sport-related TPF injuries, it is difficult to determine their frequency among the athletic population – especially since many of the studies are case studies or epidemiological reports such as:
- A case of TPF in the L1 vertebra of a trainee association footballer, resulting from an impact with the goalkeeper’s knee to the player’s back, and complicated by a traumatic transverse colon rupture requiring a stay in intensive care(9).
- A case of lumbar TPF at both L2 and L3 (confirmed on a CT scan) during an American football game caused by a ‘spear’ in the back(10).
- A case of multiple displaced lumbar TPF (L1–5) in a cricket bowler who presented with chronic lower back pain, but without any obvious impact trauma(11). The researchers concluded that the most likely explanation was repeated small stresses on the spine associated with fast-bowling.
- A retrospective study of snow-sport athletes which found 43 discreet instances of TPF injury over five years, accounting for no less than 29% of all fractures reported. In this case, the researchers argued that these injuries were likely secondary to avulsion forces caused by an intense muscle spasm following a fall impact(12).
- A 1995 review study documented 29 cases of lumbar TPF in the American National Football League(13).
- A case study described a rower with a stress fracture of the left transverse process of the third lumbar vertebra(8).
Etiology of TPF injury
As mentioned, most lumbar TPF injuries result from the impact of an external force on the lower back. This mechanism of injury usually occurs from player-to-player contact via a collision. However, a fall to the ground can generate sufficient force to cause a TPF. In a 2015 case-study paper, Matthew Gray and Paul Catterson, working in conjunction with the Freeman Hospital, Newcastle Upon Tyne, UK, and Newcastle United Football Club, documented the case of a lumbar TPF injury suffered by a soccer player resulting from an impact with the turf following an attempted overhead kick(6).In a game situation, the player attempted an acrobatic overhead-kick clearance during which he landed on his left side and lower back (see figure 1). Suffering extreme lumbar pain, the athlete discontinued play. A magnetic resonance imaging (MRI) scan the following day revealed lumbar edema, which suggested a left-sided TPF of the L2 and L3 vertebrae. A computed tomography (CT) scan done 24-hours later confirmed the initial diagnosis and revealed minor anterior displacement of the fracture at L2 (see figure 2). The impact forces generated by falling from a modest height onto turf are relatively low compared to a motor vehicle accident, yet, large enough to result in a TPF injury.
Figure 1: Soccer match fall precipitating lumbar TPF(6*)
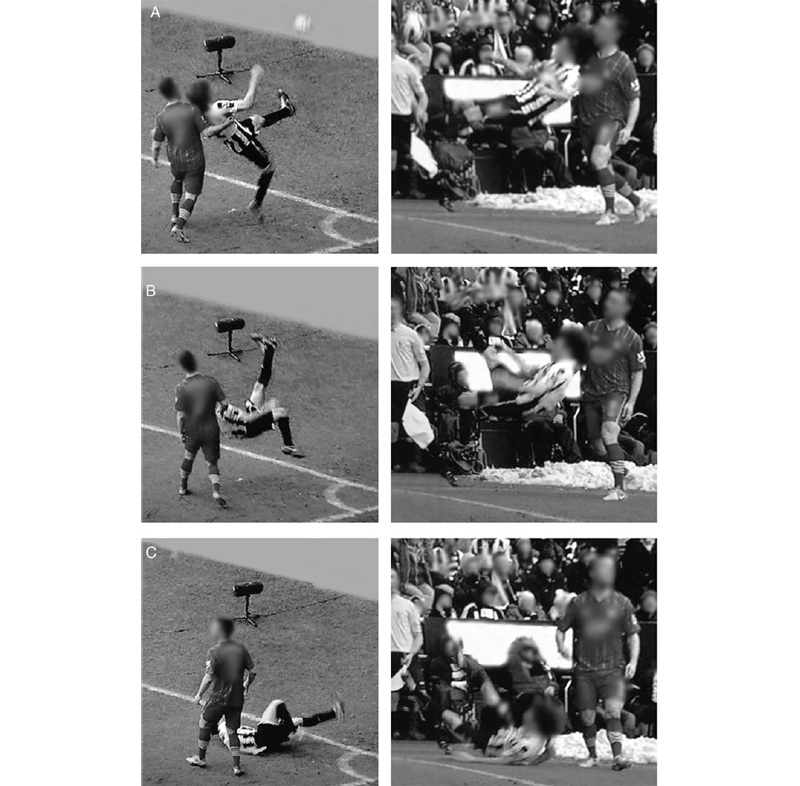
Freeze-frame capture from two angles showing the fall preceding the TPF injury. *Used with permission
When repeated over time, even smaller loadings to the spine may result in TPF injury. In the case study involving the rower cited above(8), the injury occurred while rowing in a coxless pair during a practice session. There was no reported precipitating event or trauma, yet she suffered a left L3 non-displaced stress fracture of the transverse process one month after the onset of symptoms. The researchers postulated that in the absence of trauma, the muscles and their attachments played a significant role in developing her stress fracture.
This mode of injury seems entirely feasible since, under race conditions, female rowers can generate forces in the lumbar spine approaching or even exceeding 700Newtons(14). Moreover, multiple tissues are acting on the lumbar transverse processes. In particular, the middle layer of lumbar fascia (which attaches the transversus abdominis and internal obliques) can transmit enough force to tear off the lumbar transverse processes(15,16)! This rower also developed a relative energy deficiency due to overtraining and restrictive eating habits in the 24 months before her TPF injury – a well-documented risk factor for stress fractures (see this article for a full discussion of relative energy deficiency).
Figure 2: CT scan of the lumbar spine*
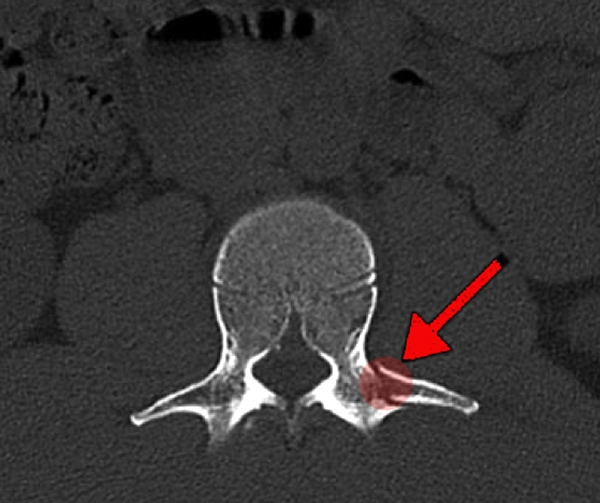
Visualized using an axial slice, showing left TPF at L2. *Used with permission.
TPF diagnosis
A TPF diagnosis relies on a combination of a physical examination to exclude other conditions that produce lower back pain, and imaging to confirm. An athlete will likely present with lower back pain that worsens with transitional movements. Spinal rotation may be particularly painful. Palpitation of the affected side may cause diffuse pain, with obvious tenderness and hypertonicity in the paraspinal muscles.To make the diagnosis, obtain a detailed history of the patient’s activities before the onset of pain – noting any possible impacts or falls. In the absence of trauma, clinicians should inquire about training loads where the athlete participates in sports with significant spinal loading – particularly whether the athlete has increased their training volume or intensity before the onset of pain. The combination of excessive training and a history of poor or disordered eating or efforts to lose weight can cause osteopenia and increase fracture risk.
With precipitating trauma to the lumbar region, clinicians need to exclude the following possible causes of pain:
- Soft tissue contusion or muscle strain
- Rib fracture
- Lumbar spine bony injury
- Pneumothorax
- Renal trauma
- Splenic trauma
- Other intraperitoneal visceral injuries
When TPF is suspected imaging can confirm the diagnosis. Plain X-ray imaging alone may miss a TPF injury(4); instead, an MRI and CT scan is preferred. MRI scans are best visualized using T1- and T2-weighted axial sequences, whereupon oedema of the bone will likely also be observed.
Management: conservative is best
Because TPFs are rarely reported and studied, the literature lacks a consensus on the appropriate management protocol. However, given that isolated TPF injuries in athletes are typically stable and not associated with neurological deficits, clinicians favor conservative treatment strategies over surgical intervention(17).Following a confirmed diagnosis of TPF, evidence suggests that the early treatment protocol should consist of oral painkillers (such as NSAIDs) along with muscle relaxants (if spasms are present) and gentle guarded movement(18). The use of a back brace during the early stages of healing may increase the athlete’s comfort. However, without evidence of instability, these devices aren’t necessary and may hamper the natural healing process(18).
Following an initial period of rest for one to three weeks, introduce low-level light activity with minimal spinal loading, such as stationary cycling. During the early stages of rehabilitation, the use of compression straps during exercise can help increase comfort. Over the next six to eight weeks, progressively increase activity levels while avoiding excessive spinal loading. If the athlete is symptom-free after eight weeks, they can resume light training that more closely reflects their typical sporting activity. Advance their activity over the next four to six weeks as tolerated. Assuming the athlete remains symptom-free, they can return to sport at that point. Some studies report faster return-to-play times than those suggested here(13), so let the individual’s symptoms and function guide their transition back to full sporting activity.
References
- J Emerg Med 2005;28:147–52
- Injury 2000;31:773–6
- Radiology 2000;215:831–4
- Clin Orthop Relat R 1996;327:191–5
- World Neurosurg. 2017;104:82-88
- Oxford Medical Case Reports. 2015; (5):288-291
- J Manipulative Physiol Ther. 2001;24(2):123-126
- Orthopaedic Journal of Sports Medicine 2020; 8(3), 2325967120910146 DOI: 10.1177/2325967120910146
- Br J Sports Med 2006;40:e6
- J Manipulative Physiol Ther 2001;24:123–6
- SMARTT 2011;3:8
- Am J Sports Med 2012;40:1750–4
- Am J Sports Med. Jul-Aug 1995;23(4):507-9
- Int J Sports Med. 2000;21(7):518-523
- Clin Biomech (Bristol, Avon). 2010;25(6):505-509
- Eur Spine J. 2007;16(12):2232-2237
- World Neurosurg Nov 2018. doi: 10.1016/j.wneu.2018.11.147
- World Neurosurg. 2017;100:336-341
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.