You are viewing 1 of your 1 free articles
Lower leg pain in athletes: know the difference
Calf pain in athletes is common, but can be tricky to diagnose. Pat Gilham looks at the various conditions responsible, and what the literature says about an effective diagnosis.
Calf muscle strain injuries are common across sports involving high-speed running or high volumes of running load, acceleration and deceleration - and also during fatiguing conditions of play or performance(1). Match-play incidences in football record 0.84 calf injuries per 100 hours, whereas rugby union risk ratios ranging from 0.98 to 5.85 per 100 hours across different playing positions(1).
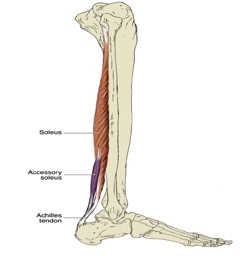
Muscle strains occur commonly in the medial head of gastrocnemius, or near the musculotendinous junction see figure 1). However, the medial third of the fibres of soleus (as well as its aponeurosis) are equally prone to injury, which is thought to be due to excessive subtalar pronation(2). The greatest risk factors for injury include an athlete’s age (rising with age), and also any history of previous injuries in this area(1). There are also associated risks with corresponding lower-limb soft tissue or joint injuries, as well as the preseason period, or the player having an increased BMI(1).
Figure 1: Anatomy of major calf muscles

Acute injury is associated with sudden localised pain, with an occasional ‘tearing’ sensation. As a rule of thumb, the degree of disability is a guide to the severity of pain experienced. Investigations are generally not required in this type of injury, although ultrasound and MRI can be useful in differentiating muscle strain versus contusion, if this is not clinically evident(3). In this instance, a comprehensive grading system based on imaging has been devised to provide diagnostic clarity in sport (see table 1)(4). It is worth highlighting that a history of persistent calf symptoms with no specific onset should alert the clinician to other possible causes.
| Grade | Symptom | Site |
|---|---|---|
| 1 |
Pain during or after activity ROM normal at 24hr Normal power and initiation Pain on contraction |
Myofascial - injury in the peripheral aspect of the muscle |
| 2 |
Pain during activity and restricts participation Limitation with ROM Pain on contraction Reduced power on testing |
Musculotendinous - Injury within the muscle belly most commonly at musculotendonous junction (MTJ) |
| 3 |
Extensive tear Sudden onset of pain Significantly reduced ROM Pain on walking Obvious weakness on testing |
Intratendinous - An injury which extends into the tendon |
| 4 |
Sudden onset of pain Significant limitation to activity Palpable gap in muscle May be less painful than Grade 3 |
Complete tear of muscle or tendon |
Potential causes of calf pain
Biomechanical overload syndrome (BOS - formerly chronic exertional compartment syndrome)
Chronic exertional compartment syndrome was first described in 1956, and was thought to be due to elevated sub-fascial or intramuscular pressure during exercise, causing hypoxia and subsequent ischaemic pain due to decreased blood flow(5).
However, a new concept refutes this claim, stating many flaws in the evidence, as well as the unreliability of the technique used for gaining intracompartmental pressure measurement(6). Instead, the phrase ‘biomechanical overload syndrome’ is preferred, and proposes the combination of muscle fatigue with poor running biomechanics as a cause of rapid tissue overload, and therefore pain. This is similar to that of upper limb occupational overuse syndrome found in musicians and office workers(6).
Onset of pain is usually insidious with running, and usually resolves when the running is stopped. MRI and ultrasound scanning will be unremarkable. Risk factors include changes in training load, or a switch of running technique to forefoot running. Lack of rest periods in training programs, as well as poor gastrocnemius and soleus capacity testing will also give strong indications for pathology. Capacity testing for soleus is best performed seated with knee angle at 90 degrees, and comparing right to left. Gastrocnemius specific testing should be performed off a step to give maximum eccentric and concentric contraction.
Cramps
The cause of muscle cramping in the calf continues to be rather obscure, although it tends to occur in less well acclimatised and conditioned athletes (2). Cramping is thought to result from alterations in spinal neural reflex activity activated by fatigue(2); contrary to popular belief however, it appears to have no relation to hydration(3). Cramps can also occur in pathologies including hypothyroidism, cirrhosis, radiculopathies, and peripheral neuropathies. It also has a strong association with inhaled long-acting b2-agonist medication and some diuretics, and a weaker association with statins(3).
Bone stress
Bone stress to the fibula and the posterior cortex of the tibia can present as calf pain(2). Stress fractures should be suspected in persons with a drastic recent increase in physical activity, or repeated, excessive activity, with limited rest and no known trauma(7). On assessment, patients usually demonstrate focal tenderness. However, this can be difficult where there is a stress fracture to the posterior cortex of the tibia, due to the surrounding muscle bulk.
A positive hop test for pain provocation can be useful as a diagnostic tool in conjunction with the subjective history, although it’s accuracy has not had recent validation(7). Similarly, applying a tuning fork to the focal pain site had 75% sensitivity, and 67% specificity in a small study(8), but is also difficult to use if suspecting a posterior cortex tibial stress fracture. MRI scanning remains the gold standard for diagnosing bone stress pathology owing to its high sensitivity and specificity(9).
Risk factors for bone stress pathologies(9)
- Female gender
- Smoking
- Consuming more than 10 alcoholic drinks per week
- Excessive physical activity with limited rest periods
- Female athlete triad (eating disorders, amenorrhea, osteoporosis)
- Low levels of 25-hydroxyvitamin D
- Recreational running (more than 25 miles per week)
- Sudden increase in physical activity
Accessory muscles
The presence of accessory muscles should be considered in the differential diagnosis of persistent calf pain once other more common aetiologies have been ruled out(10). More specifically, the accessory soleus can arise from the fibula or the deep surface of the soleus muscle, inserting onto the Achilles tendon or calcaneus. It can encroach on the posterior tibial nerve and neurovascular bundle, leading to swelling with compression and pain in the postero-medial ankle. It has a prevalence of 0.7-5.5%, and is usually unilateral in males more frequently than females(10). As shown in figures 2a and 2b, an accessory muscle can present as a soft tissue mass or swelling, and can be visualised on MRI.
Figures 2a and 2b: Accessory muscle

Baker’s cyst pathologies
Baker’s cysts or popliteal cysts that disturb the synovial fluid dynamics, and are a relatively common finding in athletes presenting with intra-articular knee pathology(11). They usually develop in the postero-medial popliteal fossa due to the lack of anatomic support in this area of the synovial capsule (see figure 3). If it dissects laterally however, this can cause compression of the popliteal neurovascular bundle.
As a result, athletes with tibial nerve entrapment (the most medial structure in the neurovascular bundle) will demonstrate gastrocnemius muscular atrophy, paraesthesia, and pain. Those with popliteal vein compression experience swelling, pain, and rarely, venous thrombo-embolism(11). In rare instances where the popliteal artery is compressed, the athlete will report lower limb claudication due to intermittent ischemia to the limb.
A Baker’s cyst can occasionally rupture, leading to calf and lower leg swelling simulating venous thrombosis. This will usually display an ecchymotic or bruised area around the malleoli(2). MRI and Doppler ultrasound imaging are most frequently used to diagnose Baker’s cyst pathology(11).
Figure 3: Baker’s cyst pathology

Neural pathology
Calf pain can be driven by neuropathic origin, particularly when the cause is a compressive neuropathy or peripheral nerve sensitisation(12). Compressional neuropathy is associated with axonal damage and demyelination, thought to be a result of long-standing compromise to nerve microcirculation at the nerve root. This can be caused by bony or soft tissue encroachment onto the nerve root in the foramen, or more commonly in the lateral recess in the spinal canal. Dermatomal pain is common; however, diagnosis is conclusive when the athlete presents with reduction of at least two out of four different domains: reflexes, muscle power, pin prick and light touch(12).
Peripheral nerve sensitisation, on the other hand, is associated with axonal neuritis rather than damage. Inflammation can be caused by acute injury to the disc tissue for example, or sometimes even direct trauma to the peripheral nerve interface itself. As a result, axonal mechanical sensitivity occurs to C and Aδ fibres when exposed to pressure -ie during neurodynamic testing(13). If an athlete presents with calf pain associated with tibial nerve sensitisation, they will present with positive slump or passive straight-leg raise testing, as well as positive pain provocation when palpating the nerve trunks of the sciatic and tibial nerves (see figure 4).
Figure 4: Nerve trunk palpation

Sciatic notch palpation

Tibial nerve palpation at popliteal fossa
Peripheral Artery Disease (PAD)
Atherosclerosis of arteries supplying the legs occurs in 3 to 10% of adults, even in fit young athletes (although less common)(3). Calf pain or claudication can be an indication of femoral or popliteal artery occlusion or stenosis, and will usually consist of muscle fatigue, aching, cramping, numbness or heaviness on physical exertion, which is relieved by rest within 10minutes.
Dorsalis pedis and posterior tibial pulses should be palpated. Absence of both pulses strongly suggests PAD, whereas the presence of either pulse makes PAD less likely (which can be normal in healthy adults anyway)(3). A positive Buerger’s test in an ischaemic leg will cause pallor at 15-30 degrees of elevation when in supine, and held for 30-60seconds. Then when returning to normal sitting position from supine, the leg colour will return much more slowly in PAD than in a normal vascularity(3)
Another useful method of diagnosis, which can be easily used in clinic is the ankle-brachial index (see figure 5)(3). Systolic pressures are taken using a pressure cuff at both arms and legs individually, and then divided to give a figure, where a normal score is 1.0-1.4. A measurement of lower than 0.9 indicates PAD(3). Doppler, and also CT angiograms are recommended investigations if PAD is suspected(2).
Figure 5: Calculating the ankle-brachial index

The figures in boxes are given as examples. Calculate using both the PT and DP pressure and use the lowest figure obtained as the overall brachial index.
Popliteal artery entrapment (PAE)
PAE is an uncommon overuse injury and is frequently caused by compression of the popliteal artery by surrounding musculotendinous structures as it exits the popliteal fossa(14). The most common occurrence involves an accessory medial head of gastrocnemius passing posteriorly to the popliteal artery. Compression can also occur, however, as a result of fibrous bands of the gastrocnemius or popliteus muscle(14).
Symptoms will be similar with that of BOS, such as calf tightness or cramping, which settles with rest. Distinguishing between the two is difficult however as aggravating factors may differ. PAE will be aggravated by non-impact activities such as cycling, swimming or walking, whereas, BOS is typically only aggravated by running(6). For an in-depth discussion of PAE, please see Chris Mallac’s article in issue 160.
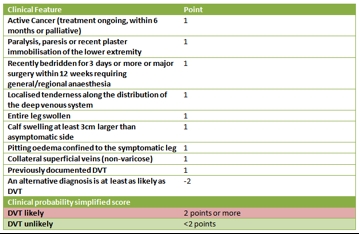
Deep Vein Thrombosis (DVT)
DVT is another potential vascular cause of calf pain, which must not be missed. Symptoms in the calf will be red, hot, firm, swollen and tender to touch(3). It usually occurs after surgery or following a period of immobilisation, but can also present in association with calf injuries. This is owing to the post-injury combination of lack of movement, disuse of the muscle pump, and the compressive effect of swelling – all of which may lead to venous dilatation, pooling and a decrease in the velocity of blood flow. Athletes who sustain calf injuries should therefore be discouraged to take long airplane flights in the days after injury(2). Diagnosis should combine emergency ultrasonography, as well as the use of the Wells score as a risk-stratification tool (see table 2)(3).
Table 2: Risk stratification for DVT using Wells score
Medication-related pathology
It is worth mentioning that statins can cause myalgia or muscle pain, particularly of the calves in 5-10% of users(3). This is interesting when taking into account recent findings, which show that professional endurance athletes, particularly females, are not immune to development of atherosclerosis(15). Symptoms start on average 1 month after statin initiation, but can be delayed for 6 to 12 months(3).
Fluoroquinolone antibiotics such as pefloxacin and ciprofloxacin, have links with predisposing those in sports participation to tendinopathy, and in extreme cases tendon rupture. This is most likely in people over 60 years of age. However fluoroquinolones are frequently prescribed for more serious respiratory tract infections, so this factor should be considered if an athlete has been prescribed such medication(16).
References
- Br J Sports Med 2017; 51: 1189-1194
- Brukner, P. in: Khan K. 2007 (3rded). Clinical Sports Medicine. Sydney. PA: McGraw-Hill Companies.
- Med Clin N Am 2014; 98: 429-444
- Br J Sports Med 2012; 46: 112-17
- Scand J Med Sci Sports 2004; 14:215-20
- Br J Sports Med 2012; 0:1-3
- Am Fam Phys 2011; 83(1):39-46
- Mil Med 1997; 162(12): 802-803
- Arthrosc Orthop Sports Med 2015; 2(2): 95-102
- The Foot 2013; 23: 154-161
- J Vasc Surg 2011; 54: 1821-1829
- Eur Spine J 2011; 20: 482-490
- Pain 2005; 117 (3): 462-472
- Sports Health 2012; 4(2): 121-127
- Plos one 2016; 11(11): 1-10
- BMJ Case Rep 2009; 1-4
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










