You are viewing 1 of your 1 free articles
Hip and groin injuries: unraveling the mystery

The hip is a major weight-bearing joint, which transfers the force and energy between the upper limb, trunk and lower limbs in order to produce movement. Walking, running or throwing cannot occur without transmitting energy through the pelvis. This means that all upper and lower body forces will impact this region and place some demand upon the muscles, ligaments and joints. This also explains why the hip/groin is thought to contribute to up to 14% of all athletic injuries(1), with approximately 30% of hip pains going undiagnosed(2).
Injuries that occur in this region can be divided into:
• Articular (bone/joint related) pathologies such as femoro-acetabular impingement (abnormal bone-to-bone contact between the femur and the acetabulum) or labral tears
• Extra-articular (meaning outwith the joint) such as muscular strains, ligament sprains, tendinopathy, or muscle weakness and imbalance(3).
This multitude of structures is what makes the hip so difficult to assess as the articular structures are very deep and are enclosed with thick layers of muscles and ligaments to provide the joint stability.
Figures 1a and 1b: Hip and groin anatomy

Fig. 1: a) Hip joint showing the femoral head (the end of the thigh bone) connecting to the acetabulum (the socket), where a tear to the labrum is detailed.
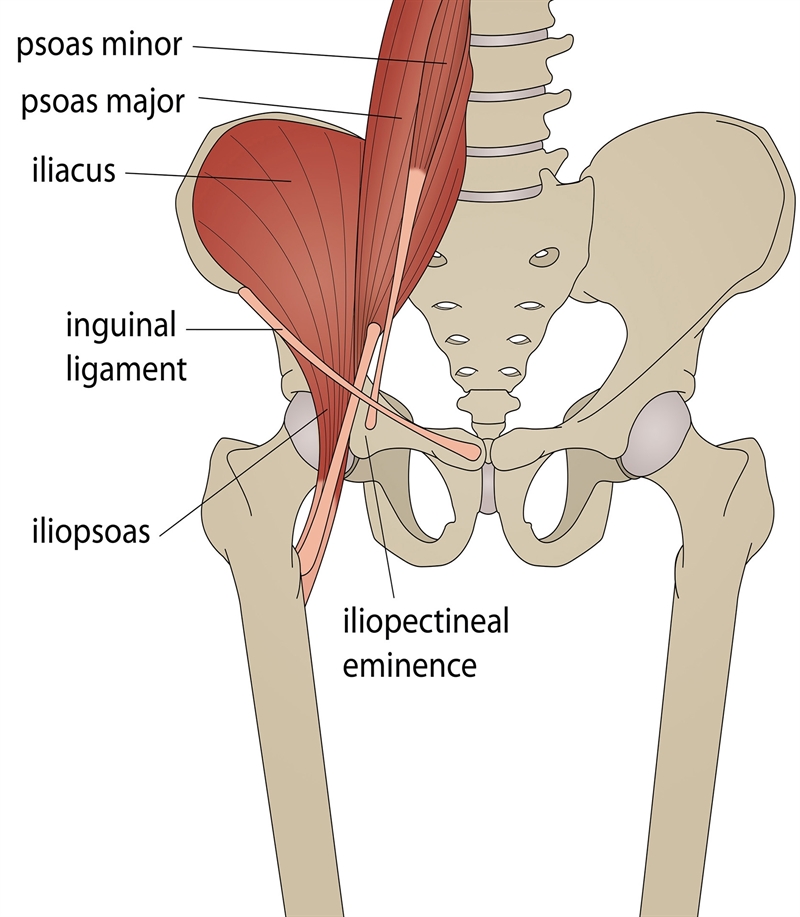
Fig. 1: b) Hip joint and pelvis with surrounding muscles shown(4).
The hip is a ball and socket joint, the ball being formed from the head of the femur and the socket by the acetabulum of the pelvis (see figures 1a and 1b). The socket depth is increased due to the fibrocartilage lining of the labrum (similar to the cartilage in the knee). This extra depth to the acetabulum holds the ball in the socket and provides inherent stability to the hip joint, along with the support of the many surrounding muscles and ligaments. The labrum also contains free and sensory nerve endings that are involved in pain perception and proprioception ie the awareness and balance of the joint within the body(5).
This architecture allows the hip to move in all three planes (forwards and backwards, to either side, and to rotate inwards and outwards) giving six different movements, making it a very versatile joint(6). This mobility however is what makes the hip joint complex in nature, with numerous other structures playing supportive roles. However, when subjected to forces during sport – eg running - this allows an array of complications.
Incidence of pathology
The hip joint is thought to contribute to up to 14% of all athletic injuries, and when there is groin pain involved 44% of these pathologies will be hip joint in origin(6). Abdominal injuries only account for 2% and adductor injuries for 1%(7). Adductor longus is the most common adductor muscle to be injured due to its long anatomical structure, and it has the longest enthesis in the body (the transitional area between the tendon and bone where there is no vascularisation and therefore delayed healing)(8).The complexity of gaining an accurate diagnosis is illustrated by the fact that around 30% of hip pathologies are not accurately diagnosed(6). Failure to clearly diagnose and treat these conditions can place the athlete at long-term risk. Initially, there’s a risk of re-injury and further damage to the hip region, but more worryingly there’s an increased risk of predisposing the hip to osteoarthritis in later years due to the repetitive overloading to the damaged cartilage(3).
Patterns of recognition
The first step towards an accurate diagnosis is to take a detailed history of the mechanism of injury and the symptoms the athlete is experiencing. Following this information, clinicians should then begin a physical examination beginning with the most likely ‘culprit’ to either confirm or rule out. Table 1 is a reference table with suggestions as to how these structures may be damaged and what symptoms might be observed.| Hip joint | Adductor injury | Abdominal injury | |
|---|---|---|---|
| How injury occurred | Repetitive flexion activitiesExcessive loading and weight bearing combined with twisting | KickingRunning with sudden speed and direction changes | Repetitive over stretching e.g. kicking and leaning backwards for the full powerExtension and rotation together |
| Signs & symptoms | Deep, vague pain that has a widespread location around the hipThe œC sign, where patients will place their hand on the outside of the hip to locate the painful site, forming a C-shapeClicking or catching sensationsLoss of hip movements and associated with pain | Deep, vague pain in adductor muscle regionLoss of kicking distanceLoss of acceleration and speed with runningPainful to change direction, roll out of bed, or to stand up | One sided abdominal painDeep, vague pain with dragging sensationPainful to cough or sneezePain on sit ups, kicking or sprinting |
Key assessment tests
There is an extensive list of diagnostic tests now being used worldwide; a full description however is beyond the scope of this article. Here, we present a couple of key tests to identify pathology in each of these regions. Remember to look at the whole picture and not draw conclusions based on these tests alone. Injuries in this region will often present with ‘overlap’, and diagnosis should be linked to your pattern recognitions, location of pain, and normal assessment of range of movement and muscle strength.Adductor related tests
1. Muscle length and toneFirst check the length of the muscle. Have your athlete lie flat on the bed and abduct their injured leg outwards as far as they tolerate. Compare this to the opposite side and note the distance moved, as well as onset of pain or any muscle guarding/tone. Repeat this test with the leg fully extended to reach the longer length muscles (adductor longus), as well as with the hips and knees bent (feet are flat on the floor to isolate the shorter range muscles such as adductor brevis). Secondly, palpate the muscle to feel for increased muscle tightness or tenderness that may suggest the source of the injury.
2. Squeeze tests
To load the adductor muscles and test for pain under contraction, have your athlete lie flat with legs extended. Place your fist between their ankles and ask them to adduct/squeeze their legs together. Then repeat this test with their hips flexed up to 60 degrees and 90 degrees to identify in which range they experience pain. At 0 degrees you are stressing mainly adductor magnus and gracilis; at 60 degrees adductor longus with maximum compression at the pubic joint; at 90 degrees pectineus and abdominal muscles are involved.
Abdominal related tests
1. Resisted sit upsTo start, have the athlete lie down with their knees bent and feet flat on the floor. Perform a normal sit up until their fingertips slide up to the top of their knees. This will raise intra-abdominal pressure, and pain may be indicative of abdominal pathology. Progress to add resistance by placing your hand over the chest. This will assess the inner range abdominal contraction against resistance, and identify if they can produce a maximal contraction.
2. Resisted rotational sit ups
To further isolate the abdominal muscles perform the same test as above; however this time have them perform an oblique sit up by twisting their trunk to one side. If they manage this you can then test against resistance. If they twist to their left you can provide resistance by pulling them to their right side and vice versa.
Hip tests
These are traditional hip assessment tests but they are very useful in identifying hip impingement pathologies. The athlete will usually complain of pain or be apprehensive about allowing you to complete the full test. To accompany these tests you should also assess general hip strength in all directions and monitor for muscle weakness and/or pain.1. FADIRS
From a supine position take the injured leg and bring the hip into full flexion, adduction and internal rotation.
2. FABIRS
From a supine position take the injured leg and bring the hip into full flexion, abduction and internal rotation.
3. Prone FABERS
Start with the athlete lying on their stomach (prone). Flex their knee upwards, abduct the leg outwards and apply external rotation. This will stretch the iliofemoral ligament (one of three ligaments that stabilise the hip joint) and reproduce their pain if it is damaged. If less than 60 degrees rotation is achieved this may be problematic as this suggests the athlete has reduced range for longer strides (for example running may place greater loading on the lower back due to restriction in the hip joint). Additionally, if there is no ‘end feel’ (ie the hip just keeps moving without restriction), this may suggest the hip ligaments are loose and the joint is unstable.
Choose your patients wisely!
Some patients will not respond to conservative treatment and early referral to a surgeon is important for successful resolution and best chance at returning to sport at the same level. If your patient presents with any of the following, you should refer them on:- Failed rehabilitation after three months, OR symptoms existing for longer than 18 months
- On-going mechanical symptoms such as limping, locking, or catching at the hip
- Poor quality of life including disturbed sleep and unable to perform sport/hobbies.
- Presence of confirmed hip osteoarthritis, or suggestive with early morning stiffness.
- Labral damage evident
- Hip internal rotation of less than 15 degrees
- Hip alpha angle less than 60 degrees (this is found on imaging and refers to an angle reported between the hip ball and socket)(9).
Early activity modification
The first step to rehabilitating these hip injuries should be education and advice on how to modify activities and lifestyle accordingly. Whilst symptoms may take time to diminish, remaining active is important for maintaining fitness. Provocative positions for the hip such as actively flexing the hip or internally rotating it should be avoided. This includes cycling, rowing, forward bending, and breaststroke swimming. Positions that load the hip joint excessively, such as deep squatting and weight bearing while rotating, should also be avoided. Prolonged sitting can also irritate the joint by keeping it flexed in a loaded position and therefore sitting duration is best kept minimal.With the onset of hip pain, other muscles will tend to become overactive in order to stabilise the joint and try to protect it from further loading. This in turn can become painful as the muscles contract further and overcompensate. Stretching and manual therapy should be used to relieve tension in the posterior gluteals, hamstrings and adductors. Hip flexor muscle strength is also found to be reduced when labral tears are present and therefore strengthening exercises should focus primarily on hip flexors to support the joint and avoid adopting altered gait patterns and hip function(10).
If an adductor injury is suspected, current research suggests early gentle movements are preferable, and to avoid specific adductor stretching for the first 48-96 hours. This rest period unloads the pubic joint and also allows the tissues to undergo early repair to withstand the contraction-induced forces without re-rupture and excess scar tissue formation(11).
Rehabilitation ideas
1. Ball squeezes with bridgesThis exercise targets the adductors initially, and by adding in the bridges, brings in the gluteals and core too. If the symptoms are acute, begin with just isometric squeezes on their own of around 10 seconds each to stimulate the adductors. Get your client to perform this with legs extended and squeeze a ball between the ankles. Also perform with ball between the knees and knees flexed. Progress to adding in the bridge exercise and increase the squeezes up to 30 seconds to provide muscle endurance.
2. Plank sequences
Planks are an excellent exercise to target the hip/adductor/abdominal region all at once. Side planks produce the maximum contraction of the gluteal muscles of the bottom leg and are one of the best ways to isolate this muscle group, giving 100% gluteal stimulation(12). Because the client is holding a plank position, the core muscles will also be recruited. Adding abduction (lifting) of the top leg will further stimulate the gluteals and adductors to counteract the muscle loads. A sequence involving the normal front planks, side planks to each side, and a reverse plank (facing upwards) with each held for 30 seconds or more will give good muscle adaptation.
3. 4-way kickers
This exercise works on improving whole hip stability of the standing leg, as well as strengthening the gluteal muscles. It is great for challenging multi-directional forces upon the stance leg and introducing unpredictable aspects of force to the stance leg. Have your client stand on the required leg with a resistance band tied around the lower legs. Kick the unaffected leg out forwards, sideways, behind and repeat this numerous times. They should ‘feel’ the stance hip muscles working to support the leg and counteract the forces being placed upon it. This should be done until fatigue is felt.
4. Hip aeroplane
This exercise also works on improving whole hip stability of the stance leg but by adding in the trunk forward flexion movement (and in the second picture the trunk rotation), core strength and stability is also challenged(13).
5. Crab walks
Have the client wrap a resistance band around the ankles and stand with feet hip distance apart. Get them to take a sideways step to the right and then bring the left leg to the right too, whilst maintaining the hip distance between legs. This will work the hip gluteals on both hips - the leading leg by abducting it, and the second leg by stabilising against the pull of the band. Repeat this sequence one way then sideways walk back leading with the opposite leg.
6. Lateral squats
These are a great progression to the crab walks above and add a dynamic element by facilitating correct hip patterns. The depth stimulates the posterior hip muscles (gluteals)(14). Get the client to stand with a wide stance and feet turned slightly outwards. Shift the weight over to the right side by bending the right knee (whilst keeping trunk upright). Then shift to the left. This can be sped up for quick reaction training.
One recipe does not fit all: treat the damaged tissue!
It is important to distinguish which structures are damaged to provide the correct principles to rehabilitation in terms of tissue loading. One prescription will not work for all injuries and will result in a delay in tissue healing, or worst scenario, could be detrimental to the tissue by loading it too severely or too frequently. Educating the athlete on these timescales is also important to gain trust and maintain motivation throughout rehabilitation.Ligament injuries require varying loads with peak isometric forces, and will see strength changes from six weeks onwards(15). Here it is important to provide contraction forces for approximately six seconds as anything greater than this will produce sub-maximal forces only and be less effective.
Tendons require sub-maximal forces with contractions of 30-45 seconds and will take 3-4 weeks for changes to become apparent. Lower level loads have been shown to produce no mechanical effect on the tendon and therefore no adaptation occurred(15). If the injury is degenerate however, it could take up to 6-8 months to observe significant improvements.
Bone injuries require a very low level load (often associated with a period of immobilisation too) but regular frequency; therefore small loads applied 4 times per day are recommended. At six weeks new callus formation occurs and by 12 weeks the bone will be strengthened.
Summary of the key points
• Dividing the hip/groin region into hip joint, adductor and abdominal pathology provides a diagnostic starting point.• Pattern recognition is crucial in beginning to understand which structures may have been injured, and to form the start of your investigations.
• Key tests to aid diagnosis include:
1) for the hip joint, the FADIRS, FABIRS, and prone FABERS;
2) for adductor injuries, muscle length and tone, and squeeze tests;
3) for abdominal injuries, resisted sit ups and resisted rotational sit ups.
• Key rehabilitation exercises include ball squeezes with bridges, planks, 4-way kickers, aeroplanes, crab walks, and lateral squats.
• There are certain patients who will not benefit from rehab. Be aware and refer on promptly.
References
1. J of Orthop and Sports Phy Ther. 1994; 19, 121-1292. J of Bone and Joint Surgery. 1999; 81B, 600-603
3. Phys Ther In Sport. 2014; May 15(2): 82-90
4. Brukner P and Khan K (2009). Clinical Sports Medicine. 3rd ed. Australia: McGraw-Hill Professional. 48-49
5. Clin Orthop Relat Res. 2008; Jan 466(1): 239-247
6. Phys Ther in Sport. 2004; 5: 17-25
7. Br J Sports Med. 2008 Oct;42(10):851-4
8. J Bone Joint Surg Am. 2007;89(10): 2173–8
9. J of Hip Preservation Surgery. 2016; 3 (3): 223–228
10. Manual Therapy. 2014; 19:405-410
11. Muscles, Ligaments and Tendons Journal. 2013; 3 (4): 337-345
12. Phys Ther in Sport. 2015; 16: 205-214
13. Journal of Bodywork & Movement Therapies (2013) 17, 266-268
14. Journal of Bodywork & Movement Therapies (2013) 17, 560-562.
15. Br J Sports Med 2015;49:278–279
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










