You are viewing 1 of your 1 free articles
Heads up: assessing and activating cervical spine ‘core muscles’
Musculoskeletal neck pain is a common complaint amongst both athletic and non athletic groups, and 67% of the population are estimated to suffer from a cervical spine disorder at some stage in their lifeMan Ther. 2004, 9: 125–133 Sports Phys Ther. 2012, 4 (4), 293 – 301. When we use the term ‘the core muscles’, it is common to refer to the core muscles stabilising the lumbar spine, due to the prevalence of injury in this area and the abundance of research available. However, the stability muscles of the craniocervical spine should not be overlooked when referring to segmental control of the spine. The purpose of this article is to explore the anatomy of the deep cervical flexors, assessment of the craniocervical spine and how decreased activity of these muscles may contribute to neck pain. We will also look at specific exercises to improve control of the craniocervical spine.
Anatomy
The craniocervical region of the neck (cranium-C2) has 40° range of movement available into flexion and extension with a further 82° in flexion and extension from the C2-T1Spine. 1998, 23 (4): 412-42. The deep cervical flexors include the longus colli and longus capitis, rectus capitis anterior and lateralis muscles.The majority of the available research has studied the activation of the longus colli and capitis, which are muscles that maintain segmental control of the spine (see figure 1). The longus capitis has three segments: the vertical fibres, the superior oblique and the inferior oblique fibres.
Figure 1: Anatomy of the longs colli and longs capitis muscles, anterior view
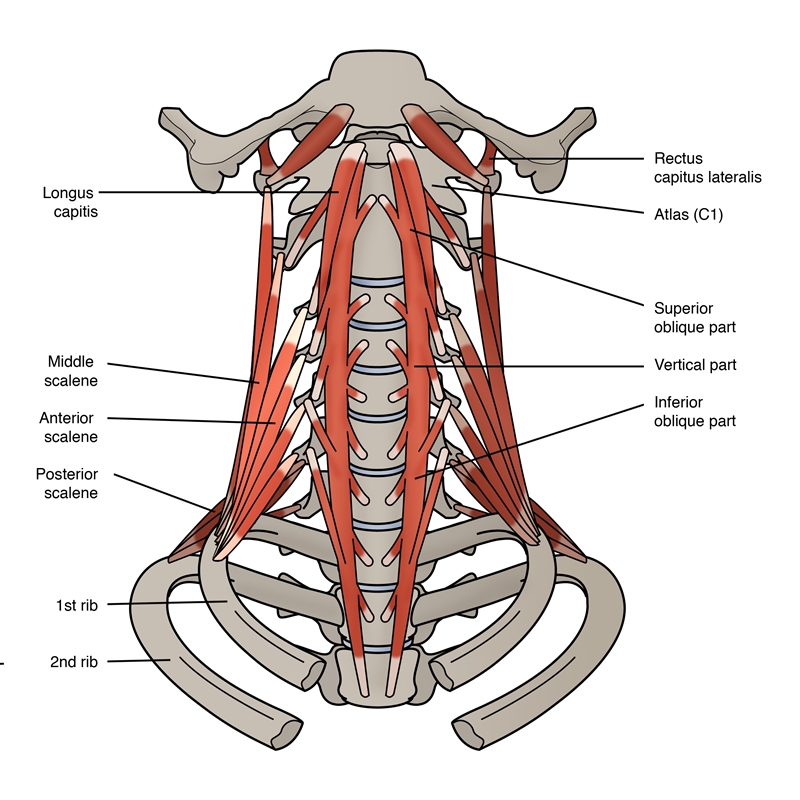
The vertical muscle originates at the anterior vertebral body T3 and inserts onto the anterior vertebral body of C1. The superior oblique fibres originate at the transverse processes of C5 and insert onto the anterior vertebral body of C1. The inferior oblique fibres originate at the anterior vertebral body of T3 and insert onto the transverse processes of C5.
Research has identified a strong association between increased muscle activity of the superficial neck flexors (sternocleidomastoid (SCM) and anterior scalene (AS) muscles) in patients with chronic neck pain, whilst also noting decreased activity of the craniocervical flexorsMan Ther. 2004, 9: 89-94. The SCM, whilst being a superficial neck flexor, is also an extensor of the upper cervical spine due to its insertion on the mastoid process. Therefore a variety of activities including road cycling, horse racing and poor technique in freestyle swimming, where extension of the craniocervical region is produced the SCM can become very dominant, and the craniocervical flexors less so.
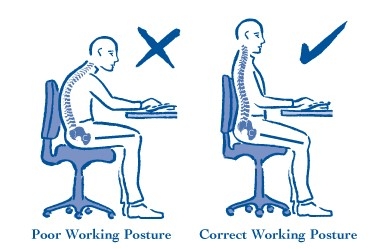
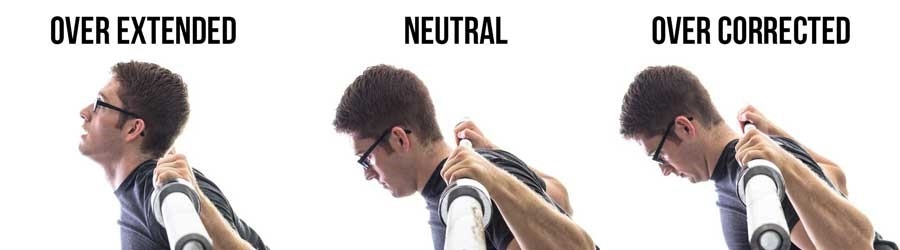
Footballers who repetitively head the ball will develop the strength of the anterior neck muscles but not necessarily the deep cervical flexors which is the desirable outcome. In addition an individual with a slumped posture whilst desk sitting, may find that they have decreased control of the deep cervical flexors and an increase in activity of the superficial flexors. This can cause an increase in upper cervical spine extension in order to still focus on a computer screen (see figure 2).
Figure 2: Positions compromising cervical spine posture, forcing upper cervical spine extension

Craniocervical Flexion Test (CCFT)
Researchers from the University of Queensland, Australia have described the CCFT, which has evolved over a 15 year periodJ of Manip and Phys Ther. Sept 2008, 31 (7), 525-533. The purpose of this assessment tool is to determine the muscle activity of the longus colli and longus capitis muscles predominately, without the activation of the very prominent SCM and AS. It should be emphasised that this test is not one of strength, as in a one rep max, but more so of precision and muscle activation timing.‘Neck pain’ is a very broad term and encompasses a wide variety of cervical spine conditions. The CCFT is a reliable test that can be used in non severe acute, sub-acute and chronic presentations of the cervical spineJ of Manip and Phys Ther. Sept 2008, 31 (7), 525-533. Contraindications to the CCFT test include any pain experienced on craniocervical flexion or referred symptoms indicating neural involvement. If present, a CCFT evaluation should cease until further investigation had taken place.
Test one
The position to measure craniocervical muscle function is as follows: the patient is positioned in crook lying with the neck in a neutral position. A thin towel may be placed under the head if necessary to maintain a neutral neck position, but a pillow is not suitable. A biofeedback cushion is positioned under the neck and inflated to 20mmHg so that the neck is resting onto the cuff but not forcing the cervical spine into extension (see figure 3). The patient is asked to perform a nodding action, without lifting their head, which would activate the deep cervical spine flexor muscles. The patient should be instructed to push their tongue against the upper palate to take away the action of the hyoid muscles. In a progressive manor the individual is asked to increase the pressure on the biofeedback unit in five stages by increasing the pressure from 20 through to 30mmHg while maintaining a hold for two to three seconds and returning to 20mmHg after each repetitionJ of Manip and Phys Ther. Sept 2008, 31 (7), 525-533(5).
Figure 3: Position for testing craniocervical flexion

During the CCFT test the clinician observes whilst also palpating for activity of the SCM and AS muscles to ensure that they aren’t dominating the exercise. The authors outlined a series of key signs that should determine the point at which a test should be ended:
- Head range of movement doesn’t increase in accordance with an increase in biofeedback unit pressure.
- Rather than a nodding action, it becomes a retraction movement.
- The head is lifted upwards (from supine lying) as if to activate the SCM and AS muscles.
- The SCM and AS muscles are active through palpation from the therapist.
- During the rest periods the pressure reader doesn’t return to 20mmHg which indicates an inability of the muscles to relax after a contraction.
Test two
Once an individual is able to achieve the 5-stage incremental test as described in test one, it is then possible to move onto the second test which involves isometric endurance of the deep cervical flexors. Again the pressure on the biofeedback unit is increased in five incremental stages of 2mmHg, from 20mmHg up to 30mmHg. The patient is asked to hold for ten seconds on each contraction, and again returning to the baseline at 20mmHg with a three to five second rest between each repetition. Indications of reduced endurance are that he/she is unable to maintain pressure at the same level, the superficial flexors become active and the movement becomes jerky (which may indicate that other muscles are actively involved). Once the individual is able to repeat each stage three times, without any of the key signs indicating dysfunction of the craniocervical flexors, the patient is asked to repeat with an increase of 2mmHg.
Research studies
Jull and colleagues found that patients with cervicogenic headaches presented with decreased muscle activity of the deep neck flexors and increased muscle timing of the upper trapezius fibers and the SCMCephal. 1999, 19 (3): p. 179-85. Patients with headache emanating from the cervical spine are frequently assessed in the physiotherapy practice and therefore the CCFT can become a useful tool for this population.The same authors also initiated the CCFT and consequently carried out a research study to determine the surface electromyography (EMG) of the SCM, AS and the deep cervical flexorsPhys Ther. 2003, 83: 899-906. They were unable to use surface EMG due to the distance from the longus colli and capitis - and of course intramuscular EMG is not a viable option due to the critical location. They therefore used surface EMG on the posterior oropharangeal wall. The researchers found that there was significant linear relationship between deep cervical flexor activation and each of the 5 incremental stages as outlined in the CCFT.
Researchers from the University of Queensland, Australia, assessed cervical and thoracic posture during a sitting computer task over a ten minute periodPhys Ther. 2007, 87:408–417. Postural analysis was measured by a marker placed on the tragus of the ear, the spinous process of the 7th cervical and 7th thoracic vertebrae and a photograph taken from a lateral view every two minutes.
Fifty eight female patients with non specific neck pain were divided into two groups: 1) craniocervical muscle training and 2) endurance strength training of the cervical flexor muscles. The exercise programmes were followed for six weeks and reassessment indicated that the craniocervical group demonstrated decreased cervical lordosis during the reassessment of the ten minute sitting computer task.
Further research carried out by the same group investigated deep and superficial neck flexor muscle activity during the CCFT and during rapid arm movements in shoulder flexion and extensionMan Ther. 2009, 14: 9-701. Forty six female patients with chronic neck pain for longer than three months were randomly assigned to either a craniocervical retraining group (as described by Jull and colleaguesMan Ther. 2009, 14: 9-701) or a strength-training programme for the cervical flexors. Both groups carried out specific exercises over a 6-week period, and all participants were reassessed at the follow up period. As in previous research described above, EMG was determined using the oropharangeal wall which was accessed through the nasal pathway.
The results revealed a significant increase in the EMG of the deep cervical flexors in the craniocervical training group where as not in the strength training group. In addition the craniocervical retraining group showed a significant effect for a decrease in EMG activity of the left and right SCM and AS muscles across all stages of the CCFT except for the 22mmHg. Furthermore, an earlier onset of EMG activity was noted in the deep cervical flexor muscles during shoulder flexion (83.5%) and extension (89%) in the craniocervical retraining group. Improvements were noted in the strength-training group but were only 55% in both shoulder flexion and extension. Both groups also significantly improved in terms of average pain intensity and the neck disability index score.
Rehabilitation
Once a patient is able to achieve good isometric endurance control using the CCFT test two, it is desirable to progress to more functional positions whilst simultaneously maintaining activity of the craniocervical flexors. The exercises shown in figure 4 provide examples of generic functional exercises which are commonly performed by a wide range of athletes, and in which the craniocervical flexors must still be used during these tasks.Figure 4: Commonly performed exercises where craniocervical segmental control is desirable
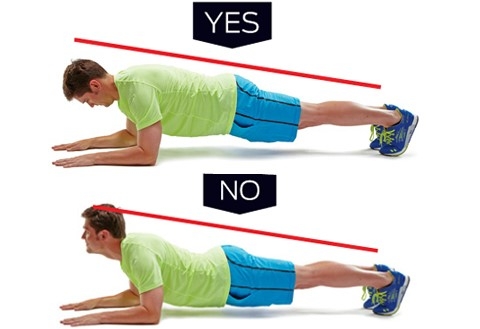


C) Start position of an abdominal crunch on the Swiss ball
For example, the plank exercise is one of the most frequently used exercises in gyms, but there is no available research that has measured the EMG activity of the stability muscles of the lower trunk or the position of the lumbar spine whilst the craniocervical spine is in extension or neutral. In such an exercise, the stability of the craniocervical spine is important.
Ideally, during a task to engage the lumbar spine stabilisers, it is desirable to emphasise complete segmental control of all regions of the spine.
| Key points |
|---|
| -The CCFT is a valid and reliable tool for measuring muscle activity of the deep cervical neck flexors and therefore can be used in patients with non severe neck pain. -The nodding ˜yes action performed in the CCFT becomes a foundation exercise for improving postural segmental control of the cervical spine as proven over a six week rehabilitation programme. |
Summary
Full activation of the deep cervical flexors is essential when managing neck pain and providing stability to the cervical spine. A number of sports and activities of daily living predispose the upper cervical region to stress and therefore the CCFT can become a useful tool in identifying aweakness in the craniocervical flexors, and then used as a treatment modality to promoting stability in this area.
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










