You are viewing 1 of your 1 free articles
Game of throws: water polo
Water polo athletes are modern-day gladiators. In part I of a series, Alicia Filley explains why stepping into the aquatic arena can be a dangerous proposition.

Water polo, while not played by the ancients, was the first team sport played in the Olympics, beginning at the 1900 games in Paris. The popularity of water polo grew, in part, due to the reckless, almost violent, style of play that delighted spectators. The pool or body of open water where it was played became a modern coliseum of sorts. This level of intense play still exists today. In a survey of injury incidence conducted by the Federation International de Natation Amateur (FINA) during the 2004 and 2008 Olympic Games, and the 2009 FINA World Championships, water polo was found to have the highest incidence of injuries, the most traumatic injuries, and the most time lost from play due to injuries1. A more recent analysis of the 2004-2018 Olympic Games and the 2009 – 2017 FINA World Championships found that 14.1 injuries occurred for every 100 players2.
Central command
Besides a swimsuit, the only required equipment worn by water polo player is a swim cap and a soft covering for the ears. The swim cap doesn’t provide protection, but rather allows players to identify their teammate. It’s no surprise then that most water polo injuries occur at the head. FINA reports that 56% of all traumas suffered by water polo athletes at the 2004 Olympic games were to the head3. Arms vie for a ball that can be thrown at speeds of up to 70 kilometers per hour by women, and faster than that by men, and the head is an easy target for both4.
Lacerations to the head can typically be tended to poolside unless they involve the cornea of the eye. Corneal abrasions can be painful and serious. Remove a player from the game, discourage him from rubbing the eye and refer to a physician if corneal abrasion is suspected. Medication to prevent infection, calm inflammation, and decrease pain may be prescribed.
Water polo athletes are also susceptible to eye irritation since they do not wear goggles. Recommend frequent use of artificial tears to prevent persistent conjunctivitis5. Chronic exposure to chlorine when wearing contact lenses can also lead to eye infections. Refer to an ocular specialist if athletes complain of irritation, light sensitivity, blurred vision, or feeling as though there is a foreign body in the eye. Advise athletes to dispose of or clean contact lenses after water sessions, or wear prescription sports lenses during play.
Blows to the head or face either from another player or from the ball itself can break delicate facial bones, affecting eyes and sinuses. In such cases, seek immediate medical attention for the athlete and evaluate for signs of concussion. If a player loses consciousness in the water, trainers must rely on other players to bring the injured player poolside. Therefore, all teams should periodically conduct life-saving drills so that players are prepared to rescue another, should the situation arise.
In a survey comparing team sports at the 2004 Olympic Games in Athens, water polo was found to have the highest number of head injuries3. In a study conducted by researchers at UC Irvine, 36% of USA Water Polo members surveyed reported suffering at least one concussion during play6. This percentage was somewhat higher for goalies5. Water polo teams, like all other sports teams, should have traumatic head injury protocols for baseline pre-season testing and return to play. Unfortunately, water polo usually falls under aquatics programming rather than field sports. Therefore, concussion protocols may be lacking. Returning to battle injured may seem heroic, but it is better to err on the side of caution and retreat until cleared by a physician.
The only protective gear a water polo athlete wears is over the ears (see figure 1). This covering lessens the trauma to the delicate ear tissue and protects the eardrum. Despite the protection, traumatic rupture of the eardrum is still prevalent and usually occurs when the ear is slapped or kicked while underwater. The resulting increased pressure in the ear canal tears a hole in the tympanic membrane. Most ruptured eardrums heal in about three months; however, they must be kept dry during the healing process. This means no pool time unless a physician approves of the use of a molded earplug and swim cap.
Figure 1: Players wearing a typical swim cap and ear covering

The other ear ailment that keeps a water polo athlete out of the water is otitis externa, commonly known as swimmer’s ear. It is an infection in the external auditory canal, brought on by one of several factors. The auditory canal becomes a perfect host for a proliferation of bacteria if it is not dried well; looses too much of the cerumen, or ear wax, or suffers a small cut. Whatever, the cause, the result is a painful condition that often comes on quickly and unexpectedly.
Treatment for otitis externa involves eardrops that usually contain an antibiotic, antifungal, and steroid suspended in an acid solution to normalize the pH of the canal. During treatment, athletes must keep the ear dry and stay out of the water. Downtime can be a week or more; thus prevention is preferable. Simple routine hygiene can prevent an earache from side-lining a water polo warrior. The use of a rinsing solution of one part rubbing alcohol to one part white vinegar as soon as players get out of the pool normalizes the pH and assists drying. Advise athletes never to insert anything into the ears to dry them. Instead, dry ears with a blow dryer on the lowest setting held at least a foot away from the ear.
Unfortunately, FINA doesn’t require mouthguards for dental protection6. As with any contact sport, players are at significant risk of dental injury. In fact, 50% of elite Swiss water polo players report witnessing a dental injury during play6. While players are free to wear the protective gear if desired, they may think that it will hinder their breathing.
If athletes complain of difficulty breathing, it may be a result of exercise-induced bronchospasm (EIB) rather than any barrier in the mouth. Common in swimmers, some evidence suggests the off-gassing of chloramines from the chlorine in swimming pools may exacerbate this syndrome5. As athletes with asthma gravitate toward aquatic activities, be aware of any athlete with complaints of shortness of breath. Simultaneous exercise-induced laryngeal obstruction (EILO) can occur with EIB and cloud the picture. Refer for further evaluation if the athlete follows their medication protocol but doesn’t show improvement. For more on distinguishing these two syndromes see Alicia Filley’s article here.
Surveillance and reconnaissance
The water polo athlete swims with his head out of the water to keep a visual on the ball and his opponents. This posture requires activation of the posterior and lateral neck muscles, which can go into spasm, causing a ‘wry neck’ or a ‘crick’ in the neck. The pain appears suddenly with a quick head turn or comes on in the morning after ‘sleeping wrong.’ The pain limits the movement of the neck and sometimes the shoulder. Treatment for a ‘wry neck’ includes ice, medication for pain, and physiotherapy. Retraction exercises are particularly effective but must be repeated hourly until pain and motion improve, usually over a few days (see figure 1).
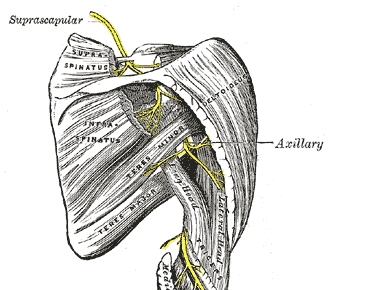
Degenerative changes can occur due to repeated hyperextension, including disc disease. Suspect disc impingement if radicular symptoms occur such as numbness and tingling in the hands. Progressive weakness may be caused by suprascapular nerve impingement. Compression or tethering may occur along the scapular spine at the transverse scapular ligament or the spinoglenoid ligament due to repeated throwing or the retracted and elevated swim stroke (see figure 2).
Figure 1: Exercises for a ’wry’ neck
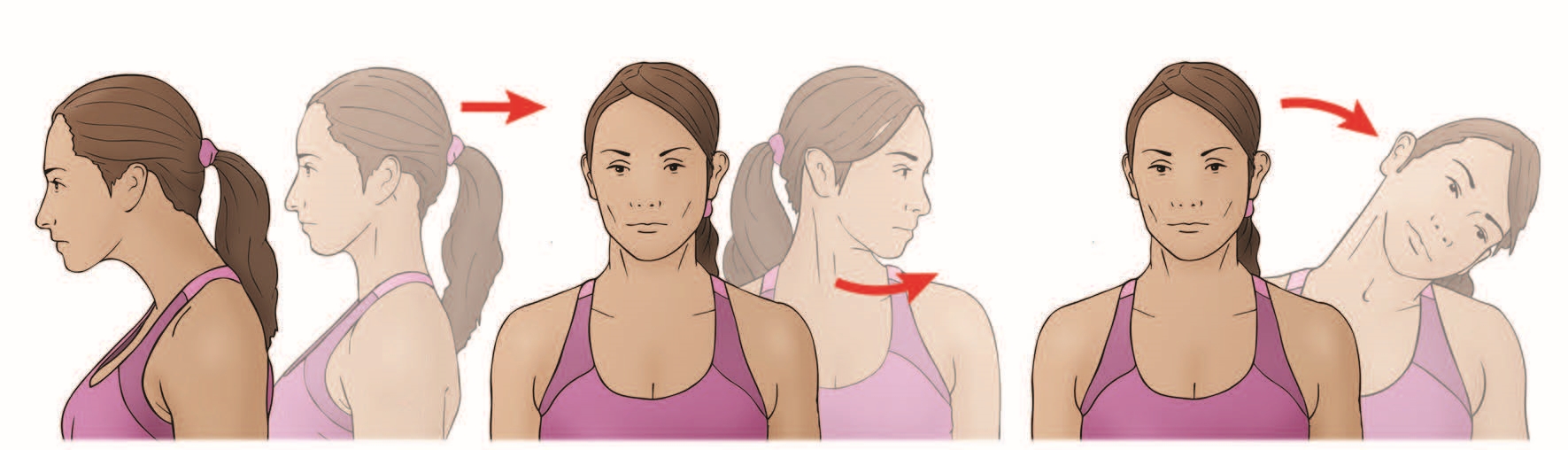
Athletes tend to guard or stiffen when suffering from neck pain. Assure them that exercise and movement are the best treatment strategies. Instruct athletes to retract their chin and hold for two to three seconds for 10 repetitions. Emphasize that the chin is retracted, not tucked. Repeat exercises every hour. When pain centralizes closer to the spine, begin retraction with rotation to each side 10 times. Progress to retraction with lateral bending, also for 10 reps each side.
Figure 2: Suprascapular nerve anatomy
Intrigue
A master of lies and deception, thoracic outlet syndrome (TOS) causes pain in the shoulder at the extremes of abduction and external rotation (a position assumed in water polo during both swimming and throwing) just as shoulder joint injuries do. However, with TOS, the pain is due to compression of the neurovascular bundle that passes through the interscalene triangle and the thoracic outlet, not from any pathology within the shoulder itself (see figure 3). Athletes with TOS may have difficulty grabbing, holding, and throwing the ball due to the weakness of hand muscles, or sensations of coolness or tingling along the arm or hand. When swimming, it may be challenging to keep fingers together during the pull phase of the stroke. In TOS there is no glenohumeral instability, however, be wary as shoulder joint pathology and TOS may exist simultaneously.
Figure 3: Thoracic outlet anatomy
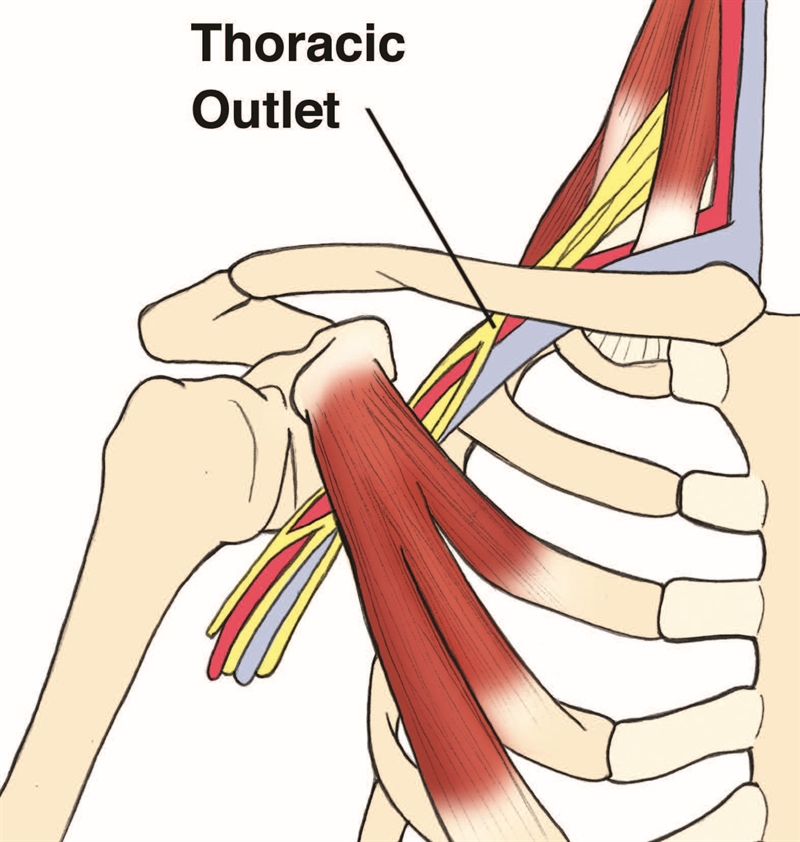
The anatomy of the interscalene triangle and the thoracic outlet. The anterior scalene muscle, the middle scalene muscle, and the first rib form the interscalene triangle, through which passes the subclavian artery, vein, and brachial plexus. Potential compression occurs at the costoclavicular space, or thoracic outlet, between the clavicle and the first rib. Researchers report various anomalies in this region, including the finding of a cervical rib, which can impinge on the neurovascular bundle7. The typical ‘swimmer’s posture’ of shortened pectoral muscles, rounded shoulders, and kyphotic thoracic spine predisposes aquatic athletes to TOS.
Diagnosing TOS depends upon a careful history and physical exam. While neither is specific for TOS, a positive Adson’s maneuver or Wright’s test, combined with a thorough history and physical exam, help distinguish TOS from a shoulder joint injury (see figure 4 and 5). Radiographs can detect the presence of a cervical rib. Conservative treatment to normalize posture and muscle length with physiotherapy and exercise usually improves the symptoms. Surgery is occasionally required to correct skeletal anomalies.
Figure 3: Adson’s test
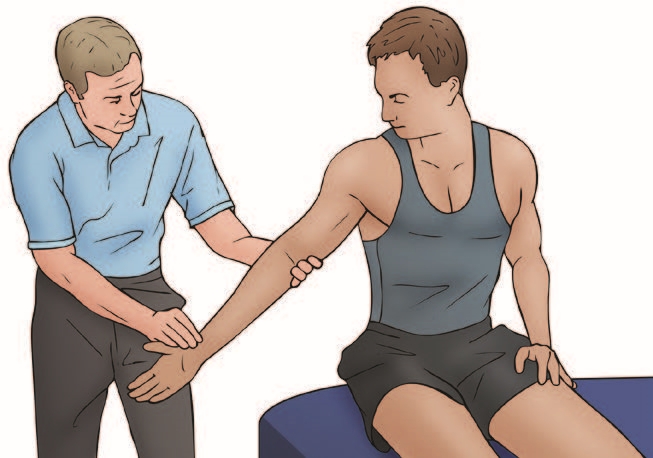
Adson’s test is conducted by finding the radial pulse at the wrist, and while continuing to monitor the pulse, moving the arm into abduction, extension, and external rotation. Instruct the athlete to take a deep breath and turn his head toward his arm. The test is positive if the radial pulse diminishes.
Figure 4: Wright’s test

Perform a Wright’s test by again finding the radial pulse at the wrist and monitoring it while moving the arm into abduction, flexion and external rotation. Have the athlete take a deep breath and turn away from the arm. If positive, this test implicates the point of compression as the costoclavicular space.
In a review of athletes treated for TOS conducted by researchers at Stanford University, 66% of the 41 competitive athletes suffered from neurogenic TOS(8). Five of these athletes played water polo. All of the subjects participated in a course of physical therapy, but due to continued symptomolgy, over half elected to have surgery. Eighty-one percent of the neurogenic TOS athletes returned to play, on average, at 4.6 months after the first rib resection and neurolysis. The 32 % of the neurogenic TOS athletes that received physical therapy treatment only also returned to competitive play. The authors suggest a course of physical therapy before surgery and conclude that athletes can enjoy excellent outcomes from both conservative and surgical treatment.
Retreat
The head and neck are the most visible body parts above the water. As such, they are easy targets for trauma and overuse. In part II of this series, Alicia Filley will explore what lies beneath, focussing on injury to the primary offensive mechanisms - the arms and shoulders.
References
- British journal of sports medicine 04/2011; 45(4):315.
- British Journal of Sports Medicine2019;53:25-31
- The American Journal of Sports Medicine 05/2006; 34(4):565-76
- J Strength Cond Res.2011 Nov;25(11):3051-8.
- Curr Sports Med Rep. 2017 Sept/Oct;16(5):363-369
- Curr Sports Med Rep.2016 Nov/Dec;15(6):410-416
- Clin Sports Med.1999 April;18(2):361
- J Vasc Surg.2014 Oct;60(4):1012-7
Further reading
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.











