You are viewing 1 of your 1 free articles
Expanding the female athlete triad: relative energy deficiency in sport affects men too
Alicia Filley explains the how energy deficiency in athletes affects performance and rehabilitation.

Sri Lanka v South Africa - 2017 Sri Lanka’s Niroshan Dickwella receives treatment and eats a banana.
The female athlete triad was long thought to be just that – a syndrome that affected only females. However, in 2014 the International Olympic Committee (IOC) released a consensus statement, which declared the female triad part of a larger disorder that included both male and para-athletes(1). The basis for this more inclusive definition was the realization that the condition was more than simply compromised bone health, disordered eating, and menstrual irregularity – the definition of the female triad. They attested that these were, in fact, among a myriad of symptoms of energy deficiency (ED).
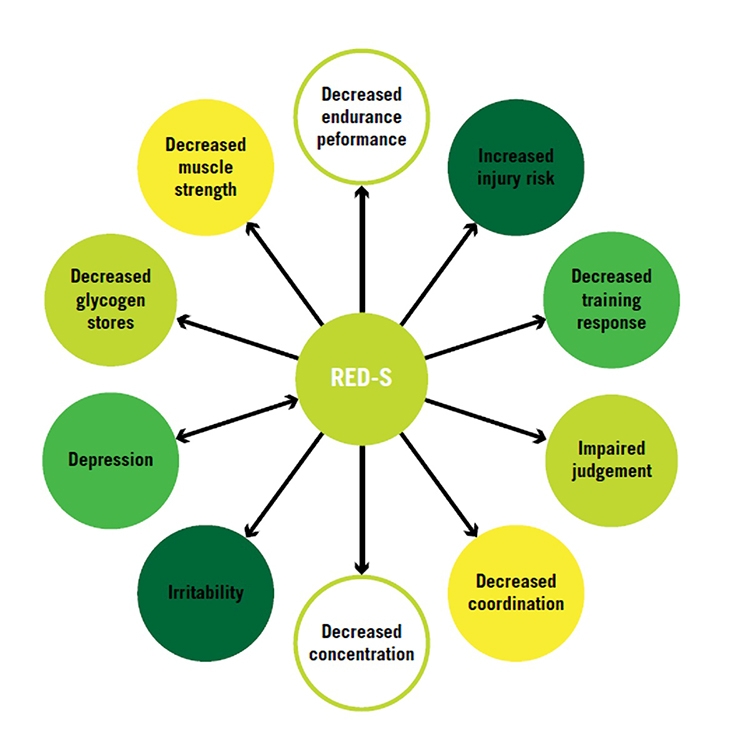
The IOC included additional possible consequences of ED in a new graphic representation of a hub-and-spokes model. This model encompassed the triad’s ‘triangular model’, and the syndrome was named ‘relative energy deficiency in sport’ (RED-S) (see figures 1 and 2)(1).
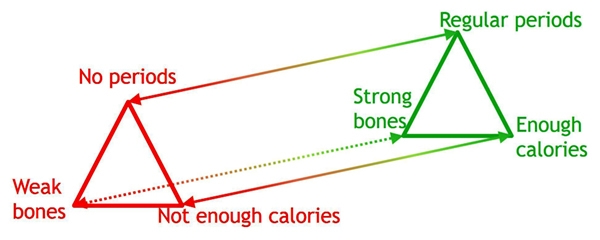
This was not the first time that energy deficiency (ED) was implicated as the cause of triad symptoms. Earlier in the triad literature, researchers pointed to low energy availability (EA) as the cause and determined that the triad symptoms were on a continuum of varying severity based on EA (see figure 3). In a rebuttal to the original IOC statement on RED-S, researchers pointed out that women experienced triad symptoms even with balanced or low EA(2). This prompted the IOC to further define the cause of RED-S as:
“The scenario termed ‘low energy availability’, where an individual’s dietary energy intake is insufficient to support the energy expenditure required for health, function, and daily living, once the costs of exercise and sporting activities are taken into account.”(3)
Figure 1: The hub and spokes model of the health consequences of relative energy deficiency in sports (RED-S)(1).
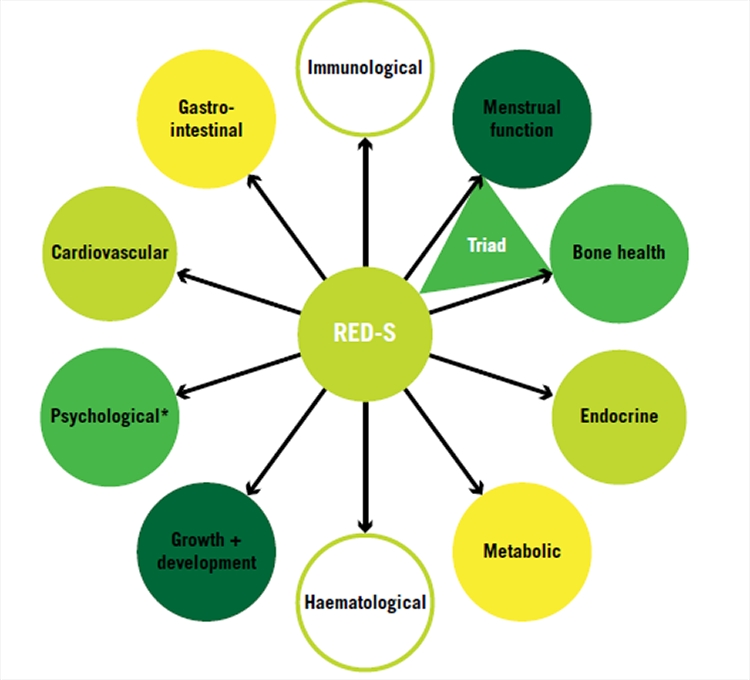
Figure 2: The hub and spokes model of the performance effects of RED-S(1).
Who’s affected?
Energy deficiency occurs when the energy required for homeostasis, daily activities, and sport exceeds energy intake. While a fairly straightforward calculation, measuring ED requires precise measurements of lean body mass, dietary intake and activity output, which are used to calculate energy availability (EA - see panel 1). If metabolic demands exceed EA, then an energy deficiency exists.
Figure 3: The continuum of symptoms of the female athlete triad
Panel 1: Formula for calculating energy availability (EA)
Calculate energy availability (EA) by subtracting exercise energy expenditure (EEE), measured in kilocalories (kcal), from energy intake (EI), also measured in kcal, and dividing that by the fat-free mass of the athlete (FFM).
EA = (EI – EEE) ÷ FFM
Example: Consider a competitive male endurance runner who weighs 70kg with 10% body fat, consumes a respectable 3000kcal diet daily, and expends 1000kcal per day in training:
- His FM is 7 kg
- His FFM is 63 kg
- Therefore, his EA is 2000kcals (3000kcal minus 1000kcal), divided by 63 kg.
- His resulting EA is 31.7kcal/kg FFM/day.
Sports research supports an EA of at least 45kcal/kg FFM/day to maintain normal physiological function and support sporting activities(4). An EA below 30kcal/kg FFM/day stresses physiological systems and compromises overall health. Therefore, in this example, the runner appears to maintain ideal body and performance parameters but may be leaching vital energy from his body.
To determine the prevalence of low EA among female athletes, researchers in Ireland conducted a cross-sectional study using an online survey(5). Out of 848 women who met the definition of being physically active, 39.6% of them were at risk for low EA. The risk was higher in those who competed in sport (76.8%) than those who were only recreational athletes.
Sports scientists at Boston Children’s Hospital administered a similar questionnaire to females seen in clinic for any sports-related injury(6). These women, with an average age of 19 years, reported they engaged in greater than four hours of physical activity per week. Survey questions evaluated the presence of disordered eating, health consequences of RED-S (such as bone and gastrointestinal health), and performance consequences. The mean BMI of the group of 1000 participants was normal. Based on the results from the eating disorder screens only, researchers determined nearly half of the participants (47.3%) suffered from low EA.
Statistics on men with low EA is sparse and sport dependent. Most agree that females are more often affected by low EA, but that is likely due to the lack of consistent data on men. It appears that males who participate in cycling, rowing, long-distance running, jockeying, and weight class martial arts are more susceptible than athletes in other sports(7).
Recognizing the signs
The human body has one objective – to stay alive. It will do whatever it takes to preserve vital organs in the face of adversity, including compromising non-essential functions. Many of the compromises in these internal systems due to low EA go unnoticed and athletes reports they ‘feel fine’.
Early detection of ED is essential to successful management(8). To detect changes and alert clinicians to the risk of RED-S, the IOC developed a screening tool called the RED-S clinical assessment tool (CAT)(9). They recommend using the RED-S CAT as part of a regular health exam or when there are visible changes in one of the physical, psychological, or performance categories affected by RED-S.
The RED-S CAT is modeled after a red, yellow and green light structure, indicating high, moderate or low risk for RED-S (see figure 4). The categorization is based on bone health, anthropometric measurements, menstrual function, endocrine health, eating, and activity habits. A green light clears an athlete for full participation in sport; a yellow light recommends participation with cautious monitoring; red excludes an athlete from participation. A similar classification determines an athlete’s readiness to return to sport after treatment for RED-S.
Figure 4: The RED-S CAT system of classification of risk for suspected relative energy deficiency in sport and continued participation in sport during treatment for RED-S.
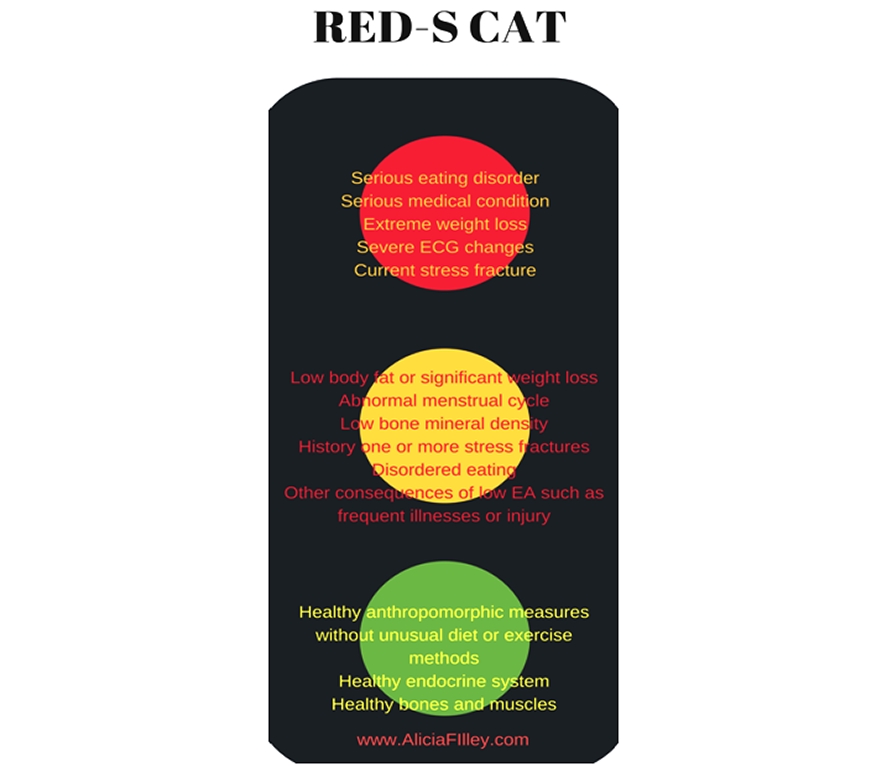
The RED-S CAT lacks validation studies but does alert clinicians when a referral for further follow-up is warranted, and when an athlete is ready to return to play.
The body can’t lie
The RED-S CAT identifies and evaluates the primary markers for RED-S. While some require medical tests, other red flags are recognizable with a thorough intake history (see table 1). The physiotherapist may be the first medical professional an athlete encounters after an injury (see figure 5). As noted in the Boston Children’s study, with nearly half of the participants at risk for low EA, every athlete, even males, should undergo a thorough screening when seen for any type of sports injury(7).
Physiotherapists often spend more time with athletes than other medical professionals. Some additional observational signs that may alert a physio to possible RED-S in an athlete are:
- Frequent injury or illness.
- Prolonged healing time.
- Over-performance of therapy or training indicating a tendency toward compulsive activity.
- Fatigue or inability to complete therapeutic activities.
- Slow gains in muscle strength or muscle wasting, despite training.
Figure 5: Simplified endocrine response in relative energy deficiency
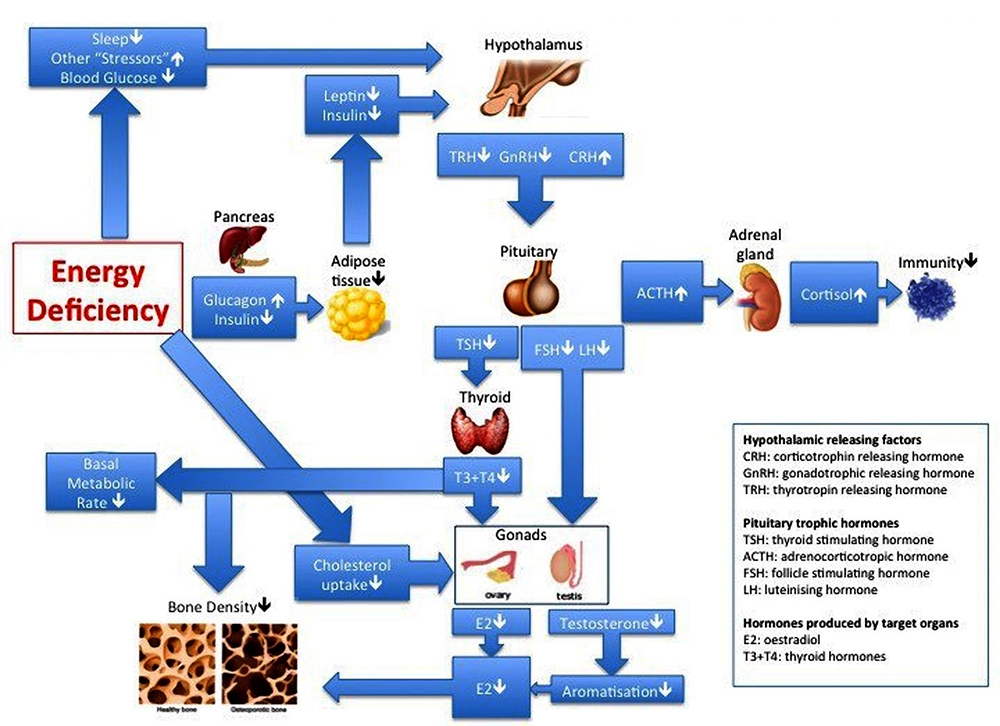
Energy deficiency affects all body systems and may be detected by a physiotherapist who notices an athlete with decreased immunity, reproductive health changes, stress fracture, or changes in cardiovascular responses to exercise. (used with permission @nickyKfitness)
Table 1: Questions practitioners can ask when assessing for RED-S.
| Menstrual history |
Have you had a menstrual period? How old were you when you had your first menstrual period? When was your most recent menstrual period? Is your cycle regular? Are you taking any form of hormones such as birth control pills, estrogen, or progesterone? |
| Eating history |
How do you feel about your weight? Are you on a special diet? Are there certain foods you exclude from your diet? Are you trying to lose or gain weight? Has anyone told you that doing so could improve your performance? Do you have an eating disorder? |
| Musculoskeletal history |
Have you ever suffered a stress fracture? Have you been told you have low bone density or osteoporosis/osteopenia? Do you have frequent tendon or muscle injuries? Does muscle soreness last for more than two days, or do you find it hard to recover from a strenuous workout? |
| Gastrointestinal history |
Are your bowel movements regular? Do you use laxatives regularly? Do you feel bloated or suffer from stomach cramps often? Do you vomit frequently? |
| General history |
Do you get colds or other illnesses often? Has your growth been along a normal developmental curve? Do you feel energized for your workouts? How many hours of sleep do you average per night? Do you feel rested in the morning? |
| Cardiovascular history |
Do you get dizzy during a workout or when you stand up? Does your heart ever race or feel like its beating slowly? |
| Mood history |
How would you describe your mood most of the time? Are you often irritable? Do you have trouble concentrating? Do you frequently feel sad or discouraged? Have you been diagnosed with depression? |
Implications for treatment
The role of the physiotherapist in the treatment of athletes with RED-S is typically the same as without: injury management. However, there are certain considerations with an athlete with RED-S. Engage with the physician, dietician, and athlete to come up with an appropriate activity strategy that addresses any current injuries, complies with the treatment plan, and keeps the athlete motivated. Incorporate bone stimulating exercises and avoid risky activities if concerned about osteoporosis or osteopenia. Address strength deficits - both those that impact the athlete’s sport and those that help with injury prevention. Monitor cardiovascular status frequently once cleared for conditioning activities. Understand the ability of an athlete to tolerate an increased training load is lower when in a state of energy deficiency, and tailor treatment accordingly (see figure 6).
The return to play period during treatment for RED-S may be the time when the athlete is most vulnerable to injury. Update the coach and trainer as to the athlete’s abilities and limitations at this time. Assess the athlete’s performance goals and make sure their work in the clinic lays the foundation to achieve those goals, yet remains within the intervention plan. Educate the athlete on the importance of periodization and recovery strategies. Address any biomechanical deficits that may also contribute to repeated injuries. Screen the athlete regularly to detect any setbacks or training errors that may lead to repeated low EA.
Figure 6: The effect of RED-S on performance compared to an athlete in an energy balanced state
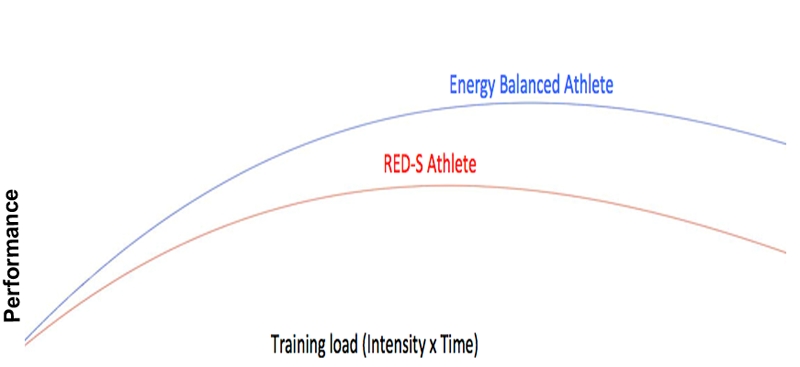
(used with permission @nickyKfitness)
References
- Br J Sports Med. 2014;48:491-97
- Br J Sports Med 2014;48:1461-65
- Br J Sports Med. 2015;49(7):417-20
- Br J Sports Med. 2018;52:687-97
- Proceedings of the Nutrition Society (2017), 76 (OCE3), E77
- Br J Sports Med. 2018;0:1-6
- Sports Med. 2016 Feb;46(2):171-82.
- Br J Sports Med. 2018;52:687-97
- Br J Sports Med. 2015;0:1-4
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










