You are viewing 1 of your 1 free articles
Chronobiology: Rhythms and Athletic Injury
We may live in a high-tech 24/7 world, but fundamental biological rhythms remain deeply ingrained in our physiological makeup. Andrew Hamilton explains how these rhythms can affect injury risk, and the implications of this for coaches and clinicians.

Humans have evolved in and are surrounded by a world full of rhythms. It would be incredible therefore if these rhythms didn’t exert a significant effect on our physiological function and performance potential, and in recent years, the field of ‘chronobiology’ has confirmed this is indeed the case.
You will no doubt be well aware of the powerful circadian (daily) rhythm. This is the most fundamental biological rhythm, regulating our sleeping and waking patterns. However, other rhythms can also impact physiological function, although the magnitudes of their effects tend to be somewhat weaker (which can make some of them rather difficult to detect against the background of environmentally induced physiological variations).
Table 1: Summary of biological rhythms.
| Rhythm | Length | Strength | Description and Examples |
|---|---|---|---|
| Ultradian | Less than 24 hours | Weak | Weaker, short-term rhythms such as 90-minute attention and alertness cycles, brain wave activity cycles, REM and non-REM phases of sleep etc. |
| Circadian | Around a day | Strong | The normal wake/sleep cycle associated with day and night; daily variations of blood pressure and temperature |
| Circatrigintan | Varies, but averages around 29-30 days | Strong | The menstrual cycle in women |
| Circannual | Around a year | Weak, but may be stronger in some individuals | Seasonal affective depression, increased risk of winter illness |
Circadian Rhythm
The circadian rhythm is the most powerful rhythm affecting humans; as well as the sleep/waking cycle, it affects hormone secretions, body temperature, mental alertness and physical performance capacity. The graphs below in figure 1 show the typical daily variations of the hormone melatonin, core temperature, levels of triacylglycerol, alertness and reaction time as a result of the circadian rhythm(1).
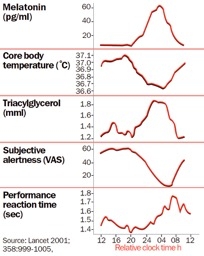
Figure 1: Daily physiological changes occurring as a result of the circadian rhythm
The pineal gland in mammals produces melatonin and regulates sleep and wakefulness (high levels induce sleep, and low levels result in wakefulness). It also synchronizes circadian rhythms, including sleep-wake timing, blood pressure regulation, and seasonal reproduction.
Triacylglycerols– are the main constituents of stored body fats in humans. Triacylglycerol levels typically rise at night to facilitate energy production in the fasted state.
As a result of these rhythmic fluctuations, many people experience maximum mental alertness, fastest reaction times and highest core temperature in the late afternoon/early evening period, while the peak in melatonin concentrations in the middle of the night period leads to maximum fatigue/sleepiness and lowest alertness. The implication of these fluctuations for sportsmen and women is that concentration, skill learning, motor skill performance, and muscular flexibility change throughout the day, and this has indeed been found to be the case.
For example, researchers at John Moores University in Liverpool looked at eight footballers’ mental and physical performance and tasks specifically related to football performance(2). Measurements of temperature (used as a marker of the body clock), grip strength, reaction times, flexibility (markers of aspects of performance), juggling and dribbling tasks, and wall-volley test (football-specific skills) were compared on different days at 08:00h, 12:00h, 16:00h, and 20:00h. The results were as follows:
- Body temperature followed the curve above (see table 1) and peaked at 16:00h (36.4 degrees C), which was significantly higher than at 08:00h (35.4 degrees C);
- Mental alertness was highest and fatigue lowest at 20:00h;
- Football-specific skills of juggling performance peaked at 16:00h, whereas performance on the wall-volley test tended to peak at 20:00h;
- Diurnal variation was found for flexibility performance tests, including sit-and-reach flexibility and spinal hyperextension. In these tests, maximum flexibility occurred between 16:00h and 20:00h, and the daytime changes in flexibility paralleled the temperature rhythms.
There are clear ramifications for athletes in terms of injury risk; firstly, since core temperature and flexibility trough in the early morning, the risk of muscular and/or ligament injury during early morning training sessions will be significantly higher than if the same workout were performed later in the day at the peak of flexibility.
This means that sportsmen and women at increased risk of injury, e.g., those who are trying regain fitness after overcoming a previous injury, or trying to rehab a previous injury, might be better off scheduling their training sessions in the late afternoon or early evening when innate flexibility reaches a peak. If this isn’t possible, then at the very least, they should consider performing an extended warm-up and moderating the workout intensity.
Another implication that flows from the circadian rhythm is that because reaction speed, alertness and motor skills tend to be diminished around the trough of the cycle, i.e., when core temperature is at minimum, the practice of sports that require fast reaction times and good coordination skills for safe execution might pose a lower injury risk if performed later in the day. So far example, when training athletes to develop fitness and skills, fitness, it may be better (where possible) for coaches to schedule fitness training sessions earlier in the day and to perform sessions where skill development or practice is the goal in the afternoon/early evening.
Medical Implications
The diurnal variations in physiology caused by the circadian rhythm also give rise to medical implications for the exercising athlete. For example, there’s evidence that lower core temperatures in the morning as a result of the circadian rhythm may actually lead to an increased risk of dehydration during exercise compared to workouts later in the day.
British researchers looked at heart rate, core temperature, sternum skin temperature, and forearm skin blood flow during exercise and a subsequent 30-minute recovery period in 12 males exercising at 70% VO2 max at 08.00h and 18.00h(3). Comparisons were made of the changes in heart rate, temperature, and skin blood flow produced by the exercise twice a day. The researchers found that the increases in core and sternum temperatures during the afternoon exercise were significantly less than in the morning, even though the workloads were not significantly different. Moreover, resting forearm skin blood flow (a measure of the ability of the body to lose excess heat) was higher in the afternoon exercise bout and the rate of change of blood flow as exercise was commenced was also higher.
There are also implications for cardiovascular health. In the general population, it’s a fact that cardiovascular events such as myocardial infarction, sudden cardiac death, and stroke have a peak incidence in the early hours after waking(4). One factor that is likely to play a role in this is the circadian rhythm of blood pressure, which peaks during the early morning period and declines to reach a minimum in the late afternoon/early evening. This explains the observation that vascular conditions such as aortic aneurysm (a rupture in the aorta) are most likely to occur during the early morning and least likely during the early evening(5).
When it comes to the cardiovascular health of athletes, there’s little specific research into conditions such as cardiac arrhythmias or the phenomenon of sudden cardiac death and their link with the circadian rhythm. However, studies on otherwise healthy adults show that cardiac arrhythmias such as ventricular fibrillation and ventricular premature beats have a much greater incidence than would be expected in the morning - during the circadian trough(6). What does this mean for coaches and therapists who have athletes in their care? For those who conduct maximal exercise testing on sportsmen and women, testing in the late afternoon might confer an extra margin of safety, particularly with older subjects or those whose exercise and medical histories are not well known.
The Circatrigintan Rhythm and Female Athletes
The powerful circadian rhythm affects 100% of the population. However, in fertile women, there’s another power biorhythm at work called the circatrigintan rhythm - more commonly known as the menstrual cycle, which typically lasts around 28 days. During this cycle, hormone levels change as the phases change; during the follicular phase (which normally occurs about 6-14 days after the onset of bleeding), there’s an increase in the circulating levels of the hormone estrogen while in the luteal phase (which begins after ovulation and normally lasts from day 15 to day 28 after the onset of bleeding), levels of the hormone progesterone rise significantly (see figure 2).

NB: LH = leuteinising hormone; FSH = follicular stimulating hormone
Figure 2: Hormonal changes during the circatrigintan rhythm
Although these sex hormones’ primary function is to enable the reproductive system to function, physiologists have long known that the fluctuating levels of these hormones can affect other functions and tissues in the body, too. One area of particular interest is the effect of sex hormones on the mechanical properties of ligaments, which is now thought to be a key factor in the greatly increased incidence of anterior cruciate ligament (ACL) injury in female athletes – compared to male athletes and females are at a 4-6-fold increase of ACL injury(7).
In a meta-study that combined data from nine prospective cohort studies, researchers investigated the association between the menstrual cycle and anterior knee laxity in female athletes(7). Three studies observed significant associations between the menstrual cycle and anterior knee laxity. These studies all reported the finding that laxity increased during the ovulatory or post-ovulatory phases of the cycle. A meta-analysis, which included data from all nine reviewed studies, subsequently corroborated this significant effect of the menstrual cycle phase on knee laxity. In particular, peak knee laxity occurred 10-14 days into the cycle (around ovulation). This laxity decreased during days 15-28 and was at its lowest during days 1-9 of the cycle.
But does an increase in ACL laxity equate to an increased incidence of injury? In another study, US researchers studied the characteristics of non-contact ACL injuries in a cohort of 83 female athletes to see whether the risk of injury was linked with the menstrual cycle phase(8). They also looked at the effect of oral contraceptive use on the incidence of injury by splitting the subjects into two subgroups: oral contraceptive users and non-users.
The results showed that there was a significant 28-day periodicity of injuries was present in the group as a whole, as well as in the two subgroups. High- and low-risk time intervals were associated primarily with late follicular and luteal phases, respectively, i.e., suggesting that ACL laxity and an increased incidence of injury are linked. There was also a significant difference in the time dependency of the number of injuries between the two subgroups: female athletes taking oral contraceptives demonstrated a greater difference in risk between the high and low-risk phases, with the high-risk phases shifted toward the beginning of the cycle.
Another US study some years later looked at anterior tibial displacement in 53 female collegiate athletes and found the following(9):
- The menstrual cycle phase did have an influence on the laxity of the anterior displacement of the knee;
- Significant increases in anterior displacement were shown during the ovulation and luteal phases of the menstrual cycle;
- Oral contraceptive users tended to have increased laxity when compared to those subjects who were not on hormone therapy.
Determining the exact risk of ACL injury in female athletes is difficult, however, because of a myriad of other variables such as individual biomechanics, training loads, and the nature of the athlete’s sport. However, it does seem that around the time of ovulation, the risk is significantly higher and is increased further in oral contraceptive users. A possible insight into the relative risk could be the measurement of a hormone called ‘serum relaxin’. A US study looked at 143 female athletes participating in sports at high risk for anterior cruciate ligament tears (basketball, lacrosse, field hockey, soccer, gymnastics, and volleyball) from 2005 to 2010(10). The results showed that elite female athletes with anterior cruciate ligament tears had higher serum relaxin levels than those without tears; those with a serum relaxin concentration greater than 6.0pg/mL had over four times the risk of increased risk for a tear. The downside of this test however is that it is not widely available.
More Recent Research
The research mentioned above(7-10)was published when studies into the circatrigintan rhythm and injury risk were relatively few. A decade later, the literature on injuries and the menstrual cycle has more than doubled, and there has been much more published research from which to draw conclusions. So, what do these later studies say?
ACL injury- In a recent systematic review on the effect of the menstrual cycle and contraceptives on ACL injuries and laxity, US researchers pooled data from 21 studies and over 68,000 subjects(11). These studies included five on the menstrual cycle and ACL injury, seven on hormonal contraceptives and ACL injury, as well as thirteen on the menstrual cycle and ligament laxity. The results showed that:
- When women were not using hormonal contraception, the luteal phase was the least associated with ACL injuries
- The two largest and highest quality studies on hormonal contraceptives and injury suggested that hormonal contraceptives may be protective against ACL injury – reducing the risk of injury by around 20%.
Ankle stability- Another recent study has looked at the increased postural sway and changes in the neuromuscular activities of the ankle stabilizing muscles at ovulation in healthy young women(12). Fourteen young women with regular menstrual cycles participated in this experiment. Postural sway and electromyographic signals of the lateral gastrocnemius, peroneus longus (PL), and tibialis anterior (TA) were recorded. At the same time, the participants performed eight different balance tasks at ovulation and early follicular phase during one full menstrual cycle.
The results showed that in the two most difficult balance tasks, significantly greater postural sway was observed at ovulation than in the early follicular phase. A similar pattern was also observed regarding PL activity, while TA activity was significantly greater in the most difficult balance task at ovulation. In addition, TA-PL co-contraction (TA/PL ratio) was significantly higher at ovulation than in the follicular phase in the two most difficult balance tasks. The researchers concluded that health professionals need to be aware of the physiological effects and the shifts in neuromuscular strategies in each phase of the menstrual cycle phase to prevent increased risk of lower extremity injury.
Skiing injuries– A study by French researchers investigated the distribution of ACL lesions according to the menstrual cycle phase in a large population of 179 female recreational skiers(13). Patients filled out a questionnaire during a consultation with the mountain physician, including the date of their last menstrual period (LMP) and contraceptive method. The results showed that 58 women (33.7%) were in the follicular phase, 63 (36.6%) in the ovulatory phase, and 51 (29.7%) in the luteal phase. Statistical analysis showed that compared with a random distribution, i.e., the menstrual phase having no effect on injury risk, ACL tears were nearly two and a half times more frequent in the pre-ovulatory than in the post-ovulatory phase. However, unlike the systematic review study above, the researchers did not note any protective effect in those women using oral contraceptives.
The Role of Proprioception and Strength
As already discussed, one possible explanation for the increased risk of injury at certain points in the menstrual cycle is increased joint laxity(7). However, some researchers have theorized that another contributing factor could be diminished proprioception. One study investigated the effect of the menstrual cycle on knee joint position sense (JPS) in healthy female athletes(14). Sixteen healthy female athletes had serum estrogen and progesterone levels assessed during the three phases of the menstrual cycle. The knee JPS was also measured during the same phases using a system comprised of skin markers, digital photography, and AutoCAD software. Absolute angular errors and changes in hormone levels were calculated between the three phases.
The results showed that the athletes had different levels of knee JPS across a menstrual cycle. In particular, JPS accuracy decreased in menses, when circulating sex-hormones levels were low. If poorer proprioception is a major factor in increasing menstrual cycle-related injuries, we might expect that female athletes would be at higher risk of injury at menses. However, numerous other studies have demonstrated that injury risk is highest in the pre-ovulatory phase, suggesting that any changes in proprioception are not significant in determining injury risk.
Another very recent study has looked at the impact of the menstrual cycle on muscular strength balance(15). In it, the researchers compared muscular balance (hamstring-to-quadriceps peak torque strength balance ratio) between the luteal and follicular phases to observe possible fluctuations in the strength balance ratio. Thirty-eight soccer athletes (26 women and 12 men) participated in two identical isokinetic strength evaluations for both knees (non-dominant [ND] and dominant [D]). Peak torque for quadriceps and hamstring muscles was measured in concentric mode, and the hamstring-to-quadriceps peak torque strength balance ratio was calculated.
The results showed that the female athletes had significantly lower hamstring-to-quadriceps peak torque strength balance ratio in the non-dominant limb during the follicular compared to the luteal phase. However, no differences between luteal and follicular phases were observed in the dominant limb. No difference in strength balance ratios was found between the dominant and non-dominant limbs in men. The potential implication of this study is that female athletes with a large strength discrepancy between dominant and non-dominant limbs might be at particular risk of injury during the follicular phase. This, in turn, suggests that efforts to strengthen the non-dominant limb in female athletes could be particularly valuable, especially in those athletes prone to knee injury.
Summary and Practical Applications
Given the association between sports injury risk and biological rhythms, what should the role of the therapist or coach be? The most important thing is to educate those in your care that natural rhythms can and do affect their risk of injury. Yes, the effects of these biological rhythms are relatively minor, but for injury-prone athletes who wish to stay injury-free, being aware of their effects could make the difference between picking up an injury before that all-important competition or staying injury-free. Here are some practical suggestions.
- Encourage your athletes to measure their own circadian rhythm peak; this is best done by measuring body temperature every two hours during a rest day, following several days of a normal, regular sleep pattern. Plot the figures and observe when the peak occurs (normally late afternoon/early evening). Likewise, female athletes can take daily temperature measurements before rising to determine the time of ovulation (indicated by a spike in temperature);
- Athletes undergoing physical rehab programs should time their sessions to coincide with their circadian peak; research suggests that late afternoon strength training produces a more favorable post-exercise anabolic hormone profile, with higher levels of testosterone and lower levels of cortisol (a hormone associated with physiological stress and muscle tissue breakdown);
- Maximal exercise testing is best performed during late afternoon/early evening (both for athletic performance and for reasons of safety);
- Encourage athletes to perform early morning workouts at a gentle pace and to warm up more thoroughly;
- Ensure that when training in hot conditions in the morning, plenty of fluid is available and encourage athletes to drink;
- Be aware that female athletes are at greater risk of ligament damage around the midpoint of the menstrual cycle and are more vulnerable to ACL injury.
- Appropriate strength training to reduce the imbalance between the non-dominant and dominant limbs may be particularly valuable for female athletes.
References
- Lancet 358:999-1005, 2001
- 2.Chronobiol Int.2007;24(3):507-19
- Chronobiol Int 2000 Mar; 17(2):197-207
- Circulation. 2004 Jun 1;109(21):2507-10
- World J Surg. 2007 Sep;31(9):1869-71
- 6.Sleep Med Rev.2011 Jun 3
- Sports Med. 2006;36(10):847-62.
- J Gend Specif Med. 2002 Mar-Apr;5(2):19-26.
- 9.J Sports Med Phys Fitness.2007 Jun;47(2):255-60
- 10.Am J Sports Med.2011 Oct;39(10):2175-80
- 11.Orthopaedic Journal of Sports Medicine 2017. 5(7), 2325967117718781
- Tohoku J. Exp. Med., 2016, 240, 287-294
- Orthopaedics & Traumatology: Surgery & Research (2013) 99, 571—575
- Knee Surg Sports Traumatol Arthrosc. 2012 Aug;20(8):1647-52
- J Sports Med Phys Fitness. 2017 Jun;57(6):859-864
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










