Tunnel vision: medial elbow pain and nerve entrapment

Medial elbow pain is a commonly reported in throwing athletes. Due to the high valgus stress put on the elbow during the throwing motion, as many as 69% of baseball players under the age of 19 report pain in this region(1). Diagnosis can be complex and the clinician needs to consider a wide variety of pathologies in this region including medial collateral ligament (MCL) strain or rupture, flexor pronator tendon strain, posteromedial impingement and cubital tunnel syndrome - to name a few.
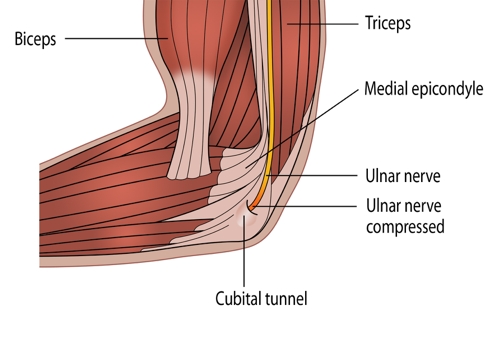
Cubital tunnel syndrome is the second most common nerve entrapment of the upper limb and occurs as a result of compression or ischemia of the ulnar nerve as it passes through the cubital tunnel (see figure 1)(2). The presence of an anconeus epitrochlearis muscle has been described as a ‘rare but possible’ cause of cubital tunnel syndrome(3-5). In this article, we will look at cubital tunnel syndrome by considering a case of compression of the ulnar nerve by the anconeus epitrochlearis muscle in a female national level waterpolo player.
Figure 1: Nerve entrapment leading to cubital tunnel syndrome
Clinical presentation
A 20-year old, right handed female water polo player presented with right medial elbow pain. She reported a 12-month history of intermittent elbow pain and burning, as well as occasional paraesthesia into her 4thand 5thdigit. She could not recall any incident/trauma to her elbow. These symptoms would be worse after national camps or tours of several weeks duration (daily water based training or games), and she would require treatment in the later stages of these tours. However, once she returned to state/club training (when water-based training was not as regular) her symptoms would resolve. Previous physiotherapy treatment had involved cervical spine mobilisation, neural mobilisation and soft tissue work. Previously these treatments had resolved her symptoms completely and she was able to return to a full training or playing load.Gradually over the course of the year however, her symptoms were becoming more regular and she was starting to get intermittent symptoms at state training and occasionally during activities of daily living (leaning on elbow). Recently she had taken three months off training (due to the removal of a benign lump in her breast). However, unlike previous episodes - where rest would relieve her symptoms - her symptoms during this time had increased.
During this time she had also commenced studying physiotherapy and her study load had increased. This included a practical component which had recently involved neural mobilisation techniques which she felt aggravated her pain. She now had pain leaning on her elbow, and felt that her grip strength had decreased, especially when using a pen or holding cup. She also reported almost constant paresthesia into her 5thdigit and ulna side of her 4thdigit.
Objective assessment
An objective assessment revealed the following:- Minor wasting of the hypothenar muscles of her right hand
- Cervical spine- slightly limited ROM and no reproduction of elbow symptoms
- Elbow – full ROM extension and flexion
- Valgus stress test of the elbow - no pain or laxity
- Ulnar nerve Tinels test - +ve
- ULNTT (ulnar nerve bias) – very limited++
- Sensation - mildly reduced light touch sensation of 5thdigit and medial aspect of 4thdigit (9/10 sensation)
At this point she was referred to sports physician who arranged investigations (see table 1).
| Investigation | Summary of results |
|---|---|
| X-ray | No abnormality detected |
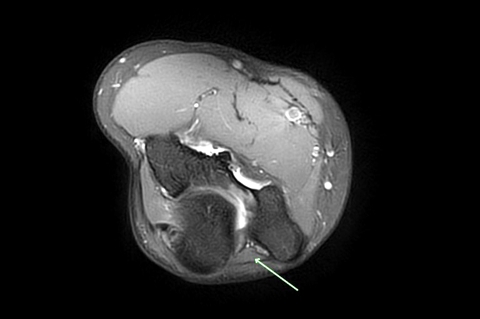
| MRI (see figure 2) | Accessory anconeus epitrochlearis muscle may be causing impingement of the ulnar nerve.No focal thickening or increased signal seen in the ulnar nerve. |
| Nerve conduction test | NAD |
Fig 2: MRI image
Following these results, she was referred to an orthopaedic surgeon for their opinion. Considering the worsening of symptoms and the lack of improvement from conservative treatment, surgery was advised. Surgery was performed a week later and the anconeus epitrochlearis muscle was excised. Intraoperatively, the surgeon assessed the stability of the nerve (once the muscle was removed) and he felt that it was stable, so no nerve transposition was required. She then followed a post-operative rehabilitation plan in preparation for returning to water polo (see table 2).
| Week Post Operative | Water polo based return to play timeline (key milestones) |
|---|---|
| Week 0-2 | Cast (back slab) at 90 degrees flexion |
| Week 2+ | Commenced active ROM and nerve sliders |
| Week 4 | Full extension (lacked 20deg elbow F)Was able to commence light swimming starting at 600m and progress distance to 2km over two weeks |
| Week 7 | Was advised by surgeon that could commence light passing however some elbow pain returned following a moderate swim session so that delayed passing |
| Week 8 | Returned to swimming with no pain |
| Week 9 | Commenced light passing; 20 passes of 5 metres |
| Week 10-12 | Elbow pain reoccurred from passing so was advised rest from passing until clinical signs and symptoms settled. Able to continue swimming |
| Week 13 | Recommenced passing 20 x 5m- 3 times per week |
| Week 16 | Commenced light shooting 20 shots at open goal 3 times per week |
| Week 17 | Shooting into goal with goalie and light wrestling in water |
| Week 18 | Full training |
| Week 20 | Returned to play domestic competition |
Physiotherapy treatment during this process involved:
- Neural sliders with a ulnar nerve bias (see figure 3)
- Lower cervical and upper thoracic mobilisation
- Soft tissue work throughout scalenes, pec minor and periscapular muscles
Load was gradually progressed dependant on clinical signs and symptoms. Symptoms were monitored via subjective questioning (pain) and clinical signs were monitored via elbow range of motion and brachial plexus provocation testing with ulnar nerve bias. If signs or symptoms worsened then training was decreased until baseline was again reached.
Figure 3: Neural sliders

Discussion
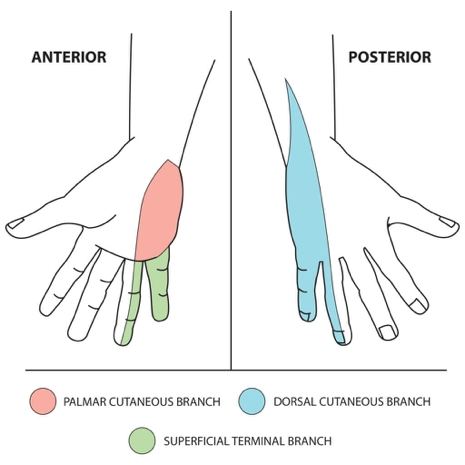
Cubital tunnel syndrome is a well-recognised compression neuropathy of the upper extremity, which causes motor and sensory symptoms in the distribution of the ulnar nerve (see table 3). As a result of this compression, patients will complain of paraesthesia or anaesthesia of the 4th(medial half) and 5thdigit, as well as weakness of the hand (especially performing fine motor tasks). Wasting of the muscles of the hypothenar eminence may also be observed(6).| Motor function | Muscles of the hand (apart from thenar muscles and the lateral two lumbricals), as well as flexor carpi ulnaris and medial half of flexor digitorum profundus. |
| Sensory function | Anterior and posterior aspect 5th digit and ulnar side of 4th digit and associated palm area (see figure 4). |
Figure 4: Sensory function due to ulnar nerve innervation
Cubital tunnel syndrome can be caused by a variety of space occupying lesions including the presence of an anconeus epitrochlearis muscle(3). The anconeus epitrochlearis is a congenital accessory muscle with a prevalence of between 4 and 34% in cadaver studies(3). It exists bilaterally in 25% of patients with cubital tunnel syndrome(1)and lies superficial to the ulnar nerve, attaching from the inferior surface of the medial epicondyle to the medial cortex of the olecranon (see figure 5 )(2).
Figure 5: Anconeus epitrochlearis
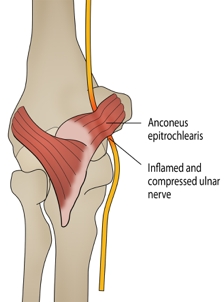
Anconeus epitrochlearis runs a similar anatomical course as the cubital tunnel retinaculum. This muscle becomes taut in flexion as well as assisting the triceps muscles in preventing ulnar nerve subluxation(4). The anconeus epitrochlearis muscle has been reported as the cause of ulnar nerve compression in 3-16% of patients with cubital tunnel syndrome in operative studies(5). Bagatur et al reported that when compared with idiopathic cubital tunnel syndrome, anconeus epitrochlearis associated ulnar neuropathy occurs at a younger age and has a more rapid progress. Also, in these patients, medial elbow symptoms are more pronounced than sensory symptoms(3). Oedema of the anconeus epitrochlearis muscle has also been noted as a feature on MRI scans(1); however this was not present in this patient.
The aim of treatment of ulnar nerve entrapment should be based not only on the relief of symptoms, but also to prevent further neurological damage. Conservative measures should always be the first line of treatment for cubital tunnel syndrome. Conservative treatment should include activity modification (throwing technique), avoidance of local pressure (leaning on elbow), avoidance of prolonged elbow flexion (narrowing of the tunnel), neural sliders and interface mobilisation/soft tissue work. Medication for the neurological pain sensation (anti-depressives and anti-epileptics) may also be considered. Usually these methods should be trialed over a 6-month period. However, if these measures fail or neurological symptoms are worsening, then operative treatment has been shown to have good outcome(1).
The surgical treatment of cubital tunnel syndrome can be divided into two broad categories(7):
- Decompressive procedures (with or without a medial epicondylectomy)
- Ulnar nerve transposition procedures (subcutaneous, intramuscular or submuscular depending on where the nerve is placed)
In cases where compression of the ulnar nerve is caused by the presence of an anconeus epitrochlearis muscle, surgical intervention has been described as either excision of the muscle or (if the nerve is determined to be unstable once the muscle has been removed) excision plus anterior transposition of the ulnar nerve(7).
Several cases surgical excision of the anconeus epitrochlearis muscle have been reported in the literature, and all of these show full resolution of symptoms and a good functional and clinical outcome(7). No previous case could be found in an elite-level water polo player. Morgenstein et al describe a case report of a elite baseball pitcher who returned to full velocity pitching at 3 months post anconeus epitrochlearis excision and ulnar nerve decompression(6). Li et al also described 3 baseball pitchers who had excision of anconeus epictrochlearis (1 of which also had medial ulnar collateral ligament reconstruction); all of these returned to their pre-injury status within one year(1).
Conclusion
Diagnosis of medial elbow pain can be complex in an overhead athlete. The anconeus epitrochlearis muscle should be considered as a potential cause of symptoms in patients with cubital tunnel symptoms. In patients with neurological symptoms who have tried conservative treatment surgical, excision of the anconeus epitrochlearis is warranted. Several case studies show that throwing athletes have all returned to pre-injury level at one year post treatment. In this case the player returned to domestic waterpolo competition after five months.References
- Orthopaedics 2012. Vol 35 No 7 e1129- e1132
- Hand Surgery 2012. Vol 17, No1 1-2
- Orthopedics 2016. Vol 39 (5) e988-e991
- Journal of Shoulder and Elbow Surgery 2009. Vol 18 e21-e23
- Turkish Neurosurgery 2014. Vol 24 No 2 266-271
- Journal of Hand Surgery 2014. Vol 41 (2) 227-228
- Clinical Rheumatology 2012. 31: 1139-1142
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.





