You are viewing 1 of your 1 free articles
Tibialis posterior tendon: a key player in foot biomechanics

The tibialis posterior tendon (TPT) is a major player in the optimal functioning of foot biomechanics, particularly as it provides stability to the medial longitudinal arch (MLA)(1). Dysfunction not only presents as pain on the inside of the lower leg and ankle, but can also be a primary cause of flat feet in the event of tendon rupture - or vice versa, with inherently flat feet causing tendon overload(2). Many health professionals are yet to fully appreciate the significance of the tibialis posterior tendon and its significant role in injury incidence, which makes it important to increase recognition of this condition(3).
Dysfunction incidence
A number of risk factors have been identified in the occurrence of tibialis posterior tendonitis dysfunction. Excess weight is a factor, with obese middle-aged women being diagnosed in 10% of cases(2). Other factors including pes planus (flat feet), steroid injections around the tendon, hypertension, diabetes and rheumatoid arthritis(3). Other causes of flat feet in adults include previous fractures, inflammatory arthropathy, osteoarthropathy, tear of the spring ligament (calcaneonavicular ligament) and tibialis anterior rupture (although this is less commonly found)(3).Triathletes often present with this injury due to the repetitive loading across the three disciplines(4). The demands on this tendon from running are obvious; with poor biomechanics, it is easy to see how the tendon can become overloaded and breakdown occurs. In swimming, the demands aren’t so obvious.
However, placing the ankle in plantarflexed position (by pointing the toes in freestyle swimming) increases the muscle shortening on the calf complex. Added to this is the repetitive pushing off the wall in pool swimming. As well as poor foot biomechanics, some of the more generic factors can cause tendon overload such as increasing training volume/load quickly, hill reps, incorrect fitting footwear(4).
During a triathlon therefore, the calf muscle shortening in the swim and the high force generation during the bike ride are combined when entering the run, which means the run begins with the calf muscles having already been loaded heavily, causing additional fatigue. Therefore effective training with proper recovery protocols is essential for preventing this kind of injury in triathletes.
Anatomy and biomechanics
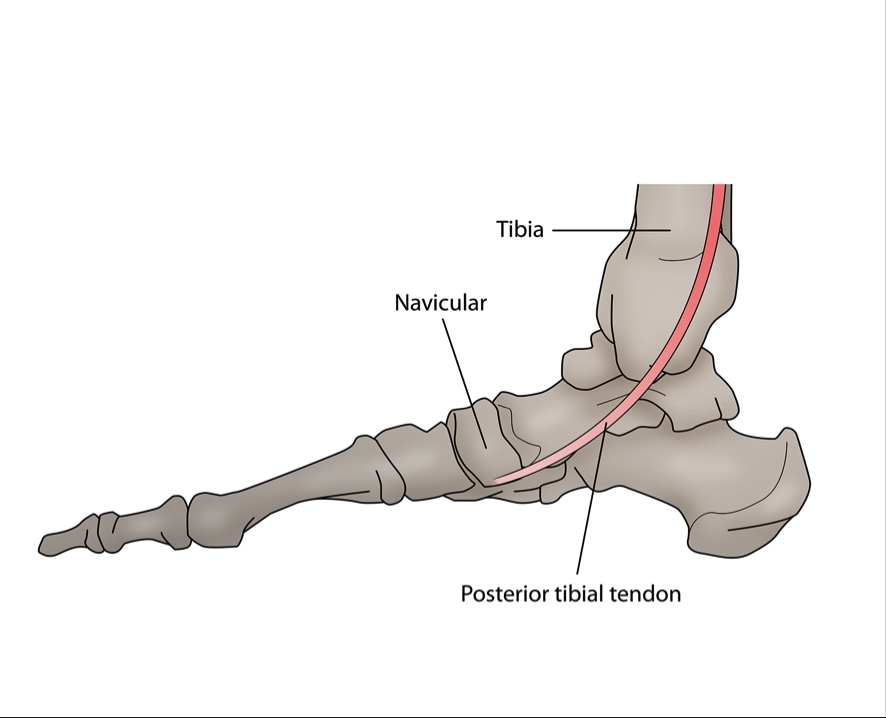
The tibialis posterior (also referred to as the posterior tibial tendon) originates from the posterior surface of the tibia on the outside aspect, with a muscular attachment on the medial surface of the fibula, and the interosseous membrane between the tibia and fibula(2). It courses through the deep posterior compartment of the lower leg, along with the more dominant calf musculature of the gastrocnemius and soleus, and passes behind the medial malleolus of the ankle. It is at this point (just behind the medial malleolus) that the blood supply is reduced(2).At the distal attachment, the tibialis posterior divides into three segments with the main section attaching to the navicular tuberosity (bony prominence) on the inside of the foot(2). The plantar segment attaches to the second, third and fourth metatarsals, second and third cuneiforms, and the cuboid bone. The third section referred to as the recurrent portion attaches to the sustentaculum tali of the calcaneus (see figures 1 and 2).
Due to the anatomical landmarks of the tibialis posterior, it is the primary ankle inverter, and also functions to maintain dynamic stability of the MLA of the foot as well as assisting the other calf muscles with plantarflexion(5). Due to its attachment sites at the navicular, calcaneal and cuneiform bones, it is evident how the tibialis posterior plays a significant role in elevating the MLA to increase the rigidity of the rear and mid foot during stance. As a result, this provides an opportunity for the gastrocnemius to function with greater efficiency(2). It can therefore be argued that the tibialis posterior tendon is of great importance in foot biomechanics.
Figure 1: Posterior view showing the TPT behind the medial malleolus
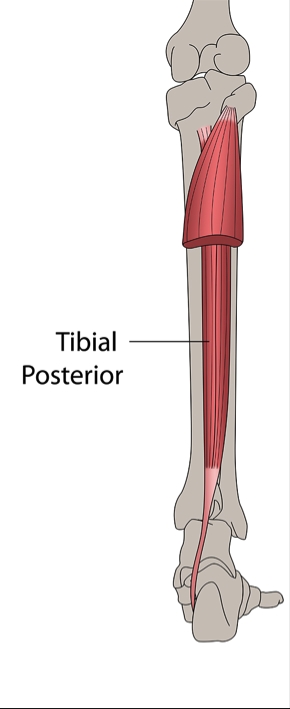
Figure 2: Medial aspect of the foot/ankle complex demonstrating the tibias posterior tendon
Pathophysiology
Quite often, tibialis posterior tendonitis will develop over a period of time - perhaps following an ankle fracture or severe ankle sprain. A significant period of time in an aircast boot or pot may result in weakness of the tendon and a reduced height of the MLA. A complete rupture of the tendon at the foot attachment does not have to occur for a flat foot deformity to occur. Therefore, a rehabilitation programme should include strengthening exercises of the foot inverters. If this strength work isn’t carried out then the tibialis posterior tendon can become exposed and repeated microtrauma can cause the tendinosis to occur.As the tendon degenerates it is replaced with fibrotic tissue, and this often occurs in areas with poor blood flow in areas such as behind the medial malleolus(2). Bubra and colleagues have stated that due to the rearfoot valgus changes, a contracture can occur of the achilles tendon resulting in changes into the forces applied at the rearfoot(2). These changes in applied forces can result in pain due to the contact of the fibula and the lateral calcaneum. A further biomechanical factor related to changes in the rearfoot is the contracture of the peroneus brevis, which causes a mechanical force applied to the opposing tibialis posterior tendon. Therefore soft tissue release should be considered for not only the tibialis posterior fibres but also the opposing peroneals.
Examination
It is essential to formulate a thorough examination protocol when you suspect tibialis posterior tendinosis may be a possibility. The first thing to assess for is any swelling behind the medial malleolus of the ankle (figure 3), which when coupled with changes in foot shape, has been found to have 100% accuracy for tibialis posterior tendon dysfunction diagnosis(3).Patients presenting with stage-one tendon degeneration typically present with vague medial foot pain on the inside of the foot, and with swelling behind the ankle(3). These patients have no history of trauma. Observe the lower leg from behind using the ‘too many toes sign’ (figure 4), which if positive indicates rearfoot valgus deformity that coincides with flattening of the MLA and compensatory forefoot abduction(2).
Figure 3: Swelling of the tibialis posterior tendon behind the medial malleolus of the ankle
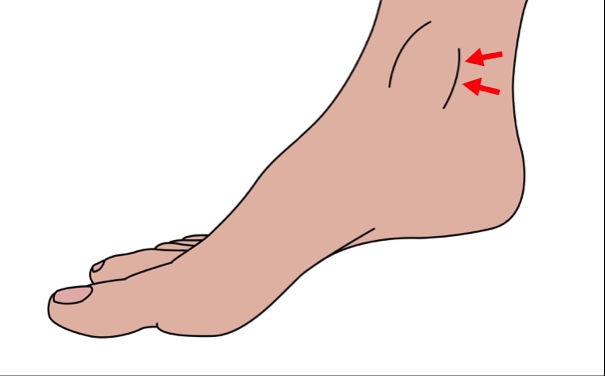
Figure 4: Too many toes sign
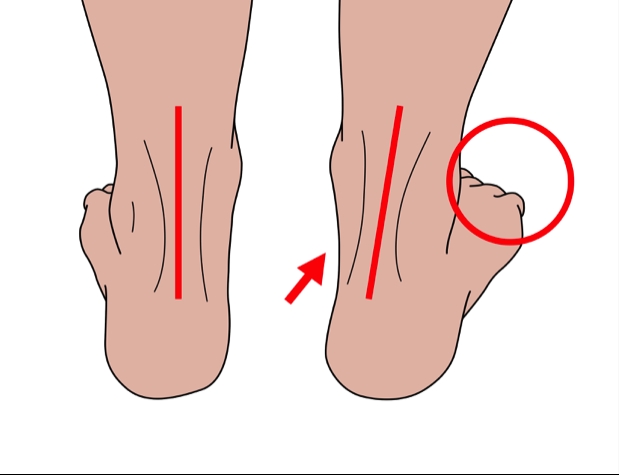
Too many toes sign as a result of the abduction of the foot, where two extra toes can be observed on the outside of the foot.
In the latter stages, there is less swelling and pain, but is more identifiable due to the single sided flat foot deformity with a valgus force of the heel bone. This leads to the ‘too many toes’ sign being noticeable. Ask the patient to raise up on their toes using both legs; an inability to do this exercise (which normally causes the heel to turn inwards) is a key indicator for tendon breakdown(3).
A progression is to ask the patient to raise up on one leg; a patient with tibialis posterior tendinosis will not be able to do this. The single-leg lift is one of the key functional tests used for this condition. If function is normal, an individual should be able to complete ten repetitions, pain free. The power of the muscle-tendon unit can be tested by resisting from a dorsiflexed/everted position into plantarflexion-inversion, which follows the actions the muscle actively facilitates(3).
An X-ray taken of both lower limbs is used to observe the patient in standing. The radiographs are best taken from the front and the outside of the ankle to best view for the presence or absence of degenerative changes in the subtalar and talocrural joints. Although a radiologist may further request an MRI scan or ultrasound scan, researchers at the Royal National Orthopaedic Hospital, UK, have argured that clinical tests for tibialis posterior tendon pain are sufficient for forming a diagnosis(3).
Treatment and management
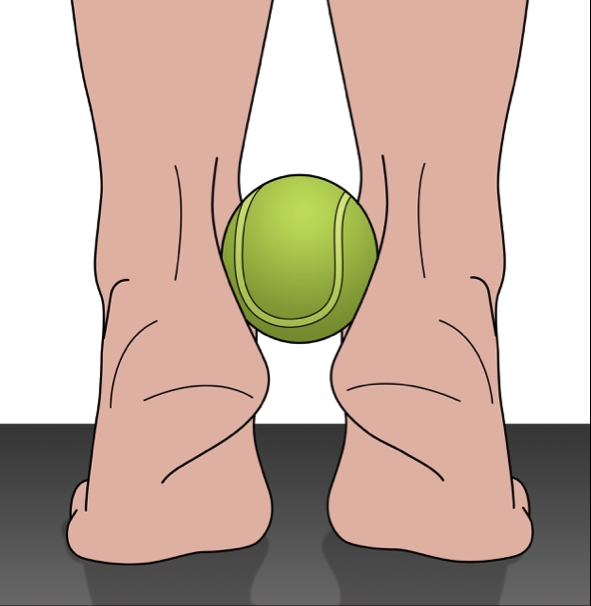
Tendon degeneration can be broken down into four different stages (table 1), and the appropriate treatment at each stage will therefore largely be dependent on the stage of injury. Stages three and four are less commonly observed in athletes, but at the same time, it is important to acknowledge the progression tendon degeneration can take.It is possible for tendon degeneration to be reversible at stage two and to correct the abnormal foot biomechanics(3). However, stage three is related to irreversible subtalar joint degeneration with irreversible tendon changes. Stage four was added to include degenerative changes within the ankle joint as well as the structures involved in stage three. It is important to develop the strength of the tendon in a functional capacity once the swelling has eased and a heel raise can be performed. A simple exercise with a tennis ball between the heels (see figure 5) helps to improve rearfoot eversion and activation of the tibialis posterior.
Table 1: Stage-by-stage presentation and conservative versus surgical management options(3)
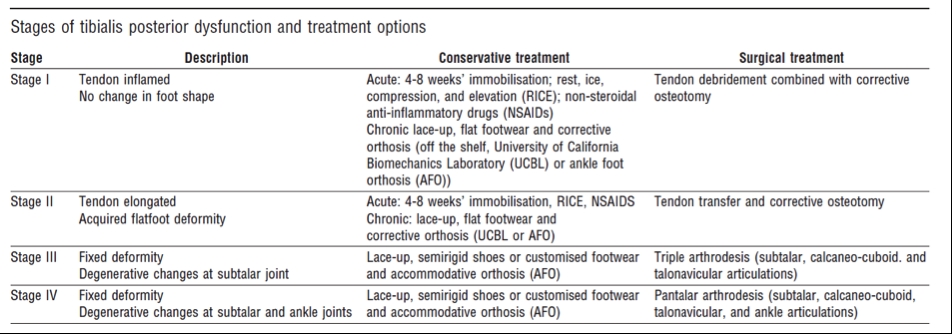
Figure 5: Double leg heel raise whilst squeezing a tennis ball actively encourages correction of the rear foot eversion.
Triathlete case study
A 41-year-old novice male triathlete presented to a physiotherapy clinic with acute right ankle pain three days after performing a flip turn during a training pool session(4). An hour into a session he felt extreme right calf pain, without a pop or snap, followed by a cramping sensation. He stopped training straight away.Pain was reported initially as 8/10 (using 0-10 pain rating scale) and presented as a dull ache. Aggravating activities included ascending stairs and driving a car. The patient had been avoiding putting any weight on his right leg. He walked with a significant limp and was unable to perform a heel raise. The patient had had previous iliotibial band, gluteal muscle weakness on the same side and was still receiving treatment for this but was almost 100% resolved.
Palpation of the tibialis posterior tendon replicated the extreme pain as did passive dorsiflexion with eversion and resisted plantarflexion with inversion. There was minimal tenderness on the medial Achilles tendon and no tenderness into the calf musculature. Furthermore, all the ankle ligament tests failed to reproduce pain. Swelling and discoloration were noted on the inside of the ankle with a girth measurement of 29cm on the involved limb compared to 25cm on the uninvolved limb.
A grade one strain of the tibialis posterior was diagnosed with treatment consisting of acupuncture, active release techniques of the calf muscles and soft tissue release using the Graston technique followed by ice and elevation. Eight days after the initial assessment the girth had reduced to 27cm and the patient was able to walk with a normal gait without a compensatory limp. After the fourth treatment (13 days after initial assessment), the pain score was two or three out of ten and he was able to ascend stairs pain free. Resisted plantarflexion with inversion reproduced minimal pain.
The patient had returned to pool training using a pull buoy to reduce load on the foot and refrained from pushing off the wall. The patient returned one month post injury and had no further aggravation of his symptoms. He was continuing the work on the bike and in the pool, plus specific tibialis posterior strength exercises with a tennis ball between the heels on a double leg heel raise.
Six weeks after the initial injury, the patient was pain free and ready to return to running. A gait analysis on the treadmill was performed, which revealed he ran with an excessive forward body lean with reduced hip and knee flexion. The patient also pronated at the ankle with significant toeing out with eversion. A single-leg squat with increased internal tibial rotation was noted with increased pronation during stance. There was also a low arch height on the right side, as indicated by a gait scan. Calluses were also noted on the metatarsal heads of both feet. Orthotics were applied along with modifications to the patients running gait. After a further month, the patient was running with an increased cadence and further distance, while remaining pain free.
Summary
A variety of conditions exist as risk factors in the occurrence of tibialis posterior tendon dysfunction, and these should be considered as a part of the examination. It is important to apply emphasis on the effective rehabilitation of ankle injuries either acutely, or following surgery, to ensure that prior injury doesn’t lead to tendon dysfunction at a later date. Effective screening should take place amongst an athletic squad to ensure that no one is present with abnormal foot biomechanics that may lead to tendon degeneration.References
- Blasimann – J Foot and Ankle Res, 2015, 8, 37
- Bubra – J Family Med Prim Care, 2015, Jan, 4, 1, 26-29
- Kohls-Gatzoulis –BMJ, 2004, 329, 1328–1333
- Howitt – JCCA, 2009, 53,1, 23–31
- Brocket – Ortho and Trau, 2016, 30, 3, 232 – 238
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.










