You are viewing 1 of your 1 free articles
Psoas major Part I: hip flexor or lumbar stabilizer?
In part I of this series, Chris Mallac looks at the detailed anatomy and function of psoas major, and the role it plays in lumbo-pelvic stability.

The anatomy and function of the psoas major (PM) has received considerable attention in the literature over the last decade. More recently however, the traditional model and understanding of the PM - and its interaction with the iliacus as being a hip muscle that contributes to hip flexion force - has been questioned. Newer models based on cadaveric and biomechanical studies suggest that the PM relationship with the iliacus is not as intimate as first thought. Its role as a dominant hip flexor may be relatively unimportant, while the notion of its primary role as a lumbar spine stabiliser has gained popularity(1).
The purpose of this two-part article therefore is to dissect the literature on the PM both in terms of its anatomy and its function, and outline the role it plays in lumbar spine stability and presenting pain and pathology in and around the lumbopelvic area.
Anatomy and biomechanics
Proximal anatomy
The PM is a long unipennate muscle that has one fascial attachment (via the diaphragm) and two fibrous attachment onto the spine (see figure 1)(2). In terms of its upper fascial attachment onto the lumbar spine and the diaphragm, the PM attaches to the diaphragm via the medial arcuate ligament. This is a tendinous arch in the fascia that covers the PM, with its fibres converging to a tendon that ascends to the diaphragm(2).
The diaphragm itself attaches to the spine via the right and left crus. They attach to the anterolateral component of the upper three lumbar vertebral bodies. The crus and their fascia overlap the PM and appear to be continuous with this muscle until they come more anterior and blend with the anterior longitudinal ligament of the spine(3). This PM-to-diaphragm attachment may have implications for lumbar spine stability as discussed later in the text.
The more traditional understanding of the proximal fibrous attachments is that the attachments of the PM are arranged as fascicles. They attach anteriorly to the L1 - L5 transverse processes (these are the posterior fascicles) and anteriorly from the T12 – L1 disc to the L4 - L5 disc (these are the anterior fascicles). The L5/S1 disc has no attachment(4).
The fiber length ranges between 3-5 cm within the posterior fascicles, and 3-8 cm in the anterior fascicles. The fascicles rotate medially so the posterior fascicles become anterior and the anterior become posterior as they descend down and laterally towards the pelvic rim(2,5). These short fascicle lengths mean that the fibre length does not extend the full length of the muscle.
Figure 1: Psoas anatomy (anterior view)

The posterior fascicles are smaller, less vertical and are located very close to the axis of rotation. As the fibres rotate medially and end up in an anterior position, these fibres now come into contact with the psoas fascia. The anterior fascicles are larger, more vertical and more suited for acting on the hip as a hip flexor along with iliacus (see function below).
The psoas minor muscle (PMI) attaches on the anterior surface of the 12th thoracic and the first lumbar vertebrae(6), and may be absent in 50% of subjects(7). Due to its absence in a large percentage of the population, it will not be discussed in this article.
Distal anatomy
The exact insertion of the PM has recently received some attention. The traditional model of the PM has been that the tendon coursed infero-laterally, and joined the iliacus tendon to form the common iliopsoas tendon, and attached onto the lesser trochanter of the femur(6,8). However, more recent research suggests that the distal anatomy may be a lot more complex than originally perceived.
The PM does not simply pass over the pelvic brim like a pulley. As it crosses the iliopectineal eminence, the fascia of the posterior fascicles attach firmly to the pelvic brim. This may constitute an innominate ligament that binds the PM to the pelvis(9). As the PM descends downwards from the lower lumbar spine levels, its infero-medial fascia becomes thick at its inferior portion and is continuous with the pelvic floor fascia(2,10). This forms a link with the conjoint tendon, transverse abdominus, and the internal oblique muscle. Again, this PM to pelvic floor fascia arrangement with the pelvic floor and transversus abdominus may have implications for its role as a lumbo-pelvic stabiliser.
Therefore, it is possible that the distal PM has many attachments. These include:
- The iliopectineal eminence (innominate ligament).
- The infero-medial fascia, which blends with the pelvic floor fascia via the PM’s inferomedial fascia (this then links with the transversus abdominus fascia).
- Anterior fibres, which may be the fibres that continue on and join the iliacus muscle.
Nerve supply
The nerve supply of PM is segmental. The anterior and posterior fascicles of PM have a separate nerve supply. The posterior fascicles are supplied by the ventral rami of spinal nerves T12 through L4. The anterior fascicles are supplied by branches of the femoral nerve from L2, 3 and 4(2). This segmental innervation may be analogous with the lumbar multifidus muscles, which have been shown to have separate functional roles in spinal stability(11).
Fiber types
There are disagreements in the literature about whether the PM muscle is mostly composed of slow-twitch or fast-twitch fibers. It was originally believed that the PM muscle had a heterogeneous distribution of fiber types across the muscle(12-14). However, further cadaver studies that enable an analysis of the entire PM muscle have shown that the size of the muscle fibers and the distribution of the muscle fiber types vary according to location(15,16). Differences can be found with regard to the superficial or deeper parts, as well as the proximal or distal parts of the muscle(17-19).
In a more recent study, Arbanas et al (2009) explored the differences in the fiber type composition of the PM muscle between its cranial and caudal portion(20). They found that the fiber type composition of PM changed from the cranial towards the caudal part of its origin. The percentage of type I fibers had a decreasing trend (less type 1 fibers around the distal part of the muscle), whereas the percentage of type II fibers had an increasing trend (more type 2 fibers distally).
Based on these findings the authors suggested that the distal part of the PM could have a dynamic role whereas the proximal portion may have more of a postural role. This fits with the descriptions of the posterior PM having more of a stability role and the anterior fibers having more of a mobility role at the hip(2).
PM biomechanics
The function of the PM is another area of controversy and uncertainty. From the available literature on PM function, it appears that the PM may have both important dynamic and postural functions. Some of the key points in the extensive literature on PM function are as follows:
- About half a century ago, Basmajian and Greenlaw (1968) argued that psoas and iliacus could not be expected to have a different function, and inferred PM activity from iliacus electromyography (EMG)(21). Since then, it has been shown that the two muscles ‘’have individual and task specific activation patterns’(22).
- The issue with EMG studies is that authors still infer PM function from surface EMG in the groin. The PM muscle is too deep to analyse with surface EMG.
- If the PM does indeed blend with the iliacus anteriorly, then it is the only muscle that connects the lumbar spine and lower limbs, and it therefore acts on both the lumbar spine and lower limb.
- The traditional view on PM function was that the PM acts as a hip flexor and may assist in lateral rotation and abduction of the hip joint(4, 23, 24). It does appear that PM contributes to hip flexion, but is not the primary hip flexor. Iliacus is more active than PM during hip flexion(25). However, it should be appreciated that rectus femoris, tensor fascia latae and sartorius are more efficient hip flexors than ilacus(26).
- It has long been argued that PM can create lumbar spine extension(21, 27). However, the biomechanics of PM suggest that it has minimal capability to produce movement at the lumbar spine (2,4,27,28).
- PM crosses the sacroiliac joint hence must create a force there. Although PM is generally thought to anteriorly rotate the innominate(29, 30), a newer model suggests that PM has the potential to posteriorly rotate the innominate in the erect posture due to its attachment onto the iliopectineal eminence(31).
- Yoshio et al concluded that the PM contributed very little to hip flexion and its primary role was for hip stability(32). This was accomplished through axial shortening, which maintained the femoral head in the acetabulum. They found that increased lumbar stability was achieved through greater angles of hip flexion.
- PM may act as secondary lateral flexor of the lumbar spine(33, 34)and contralateral trunk rotation(34).
- It has been suggested that a strong PM may be an advantage in sports that require strong hip flexion such as kicking movements and during sprint running, where fast and forceful hip flexion generates the action of the trailing leg(35, 36).
- More recently it has been suggested that PM may contribute to general stabilisation of the lumbar spine(8,34,37-40), and that contraction of the PM increases the compression forces on the lumbar intervertebral discs(37). The primary force is axial compression, which may create segmental stiffness(41)and resist shear(42).
PM as a lumbo-pelvic stabiliser
Due to the unique anatomy of the PM as described in box 1, it is possible that the PM has both a hip flexion role (anterior fascicles) and a very important spine stabilisation role (posterior fascicles)(2). PM has intimate anatomical attachments to the diaphragm and the pelvic floor. This unique anatomical location allows the PM to act as a link between these structures and may help in maintaining the stability of the ‘lumbar cylinder’ mechanism.
There is growing evidence showing how these muscles coordinate their activity to stabilise the spine. It has been shown that the transversus abdominus co-contracts with the diaphragm(43), the pelvic floor(44, 45)and the deep fibres of lumbar multifidus(11). According to this model, the PM is ideally located to assist in a stabilising role.
An extremely useful analogy to describe trunk stability is the ‘cylinder effect’ created by all of the associated muscles (see figure 2). The top of the cylinder is the diaphragm, the bottom is the pelvic floor and the middle is the transversus abdominis muscle, with the thoracolumbar fascia. PM is ideally suited to act as a link between the top and bottom of the cylinder through the medial arcuate ligament to the diaphragm and the PM fascia to the pelvic floor.
Figure 2: The cylinder effect
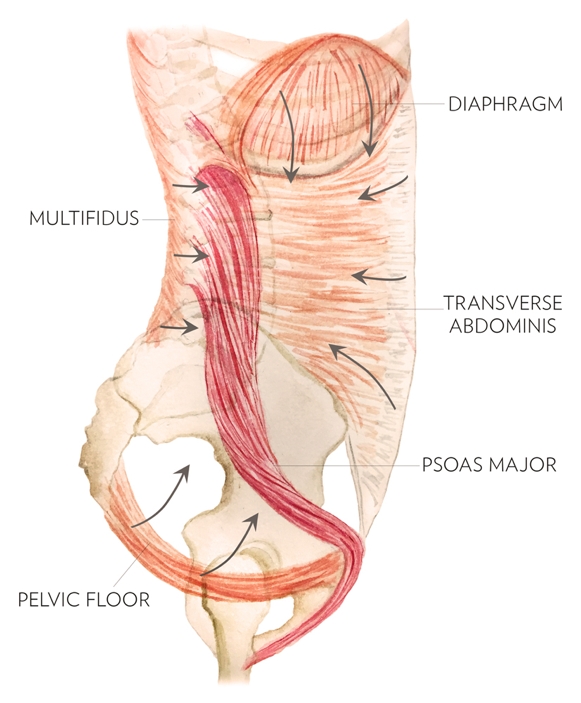
The diaphragm, pelvic floor, transversus abdominis muscle and multifidus act as cylinder walls, while PM acts as a link between the top and bottom of the cylinder.
This kind of mechanical stability is used in engineering. The placement of a rod in a cylinder will resist displacement in all directions(2, 46). In the PM analogy, this can be thought of conceptually as a supporting rod in the middle of the cylinder. Early biomechanical literature suggested that the PM might aid in the stabilisation of the lumbar spine through its large potential to generate compressive forces, which would result in increased spinal stiffness(47).
McGill 2002 conceptualizes lumbar spine stability as a fishing rod placed upright and vertical with tensioned guy wires attached at different levels along its length and those guy wires being attached to the ground in a circular pattern(42). Here the rod represents the lumbar vertebrae and the guy wires are the various muscles attaching to the lumbar spine. Reducing the tension on one of the muscles (wires) will allow the spinal segment (rod) to buckle and allow spinal injury to occur.
Juker et al (48) showed that the PM counteracts the action of iliacus during hip flexion(48). They believe that the iliacus would torque the pelvis into anterior pelvic tilt and that the PM works against these forces, adding to the stiffness within the pelvis and the lumbar spine. An activated and stiffened PM will contribute some shear stiffness to the lumbar motion segment(49, 50). This last point poses an interesting question. Does the PM contract to create hip flexion or does it contract to counterbalance the anterior tilt force imposed by contraction of the other hip flexors?
In summary
The PM should be regarded as having a very unique and ingenious anatomical design. It allows the spine to remain stiff and stable via its compressive effect on the spine and due to its contribution with other ‘core’ muscles to maintain the internal ‘balloon’ effect in the abdominal wall. Furthermore, it may contribute to hip flexion, as well as maintaining pelvic stability during hip flexion to prevent the anterior tilt drag effect created by the other hip flexors. Clearly when the demands of the hip and pelvis are increased during high-level sport function, this mechanism will automatically augment stability in the lumbopelvic region along with a greater contribution from the more superficial abdominal wall muscles. In the next article, pain and dysfunction in the PM will be discussed, and retraining of the PM muscle in the light of its functional requirements will be explored.
References
- Manuelle Therapie. 2007. 11:177-187
- Proceedings of: 11th Annual National Orthopaedic Symposium. “The Tragic Hip: Trouble in the Lower Quadrant”. Nov 6-7 1999, Halifax, Canada.
- Arch Phys Med Rehab. 1994; 75:703–708
- Clin Biomech, 1992. 7:109–119
- Proceedings of: 4th Interdisciplinary World Congress on Low Back Pain. November 9-11 2001, Montreal, Canada.
- Williams PL (1995) Gray’s Anatomy: The Anatomical Basis of Medicine and Surgery. Edinburgh: Churchill Livingstone.
- Rickenbacker J, Landholt AM, Theiler K (1985) Applied Anatomy of the Back. Heidelberg: Springer.
- Bogduk N and Twomey LT (1997) Clinical Anatomy of the Lumbar Spine and Sacrum. London: Churchill Livingstone.
- Orthopaedic Division Review. 2002. Jan / Feb: 7-16
- Williams PL, Warwick R, Dyson M and Bannister 1989 Gray’s Anatomy 37th ed. Churchill Livingstone, Edinburgh
- Spine 2002. 27(2):E29-E36
- 1992. 97, 77–81
- Acta Radiol. 1993. 24, 16–19
- Z Morphol Anthropol. 2002. 83, 305–314
- Clin Physiol. 1989. 9, 333–343
- Acta Physiol Scand. 1983. 117, 115–122
- Anat Rec. 1982. 203, 451–459
- J Neurol Sc. 1984. 63, 85–100
- J Anat. 1999. 194, 355–362
- Anat. 2009. 215, pp636–641
- Anatomical Record. 1968. 160, 310–311
- Scand J Med Sci Sports. 1995. 5:10-16
- Walther DS (1981) Pelvis and thigh muscles. In Applied Kinesiology, Vol. I, pp. 302–305
- Clin Anat. 1999. 12, 264–265
- Scand J Med Sci Sports. 1995. 5:10–16
- Physical Therapy. 1986. 66(3):351-361
- Orthopaedic Clinics of North America. 1977. 8(1):193-199
- Journal of Biomechanics. 1995. 28:339-345
- Journal of Orthopedic Medicine. 1991. 13(2):34-40
- Spine: State of the Art Reviews. 1995. 9(2):419-432
- Proceedings of: 1st International Conference on Movement Dysfunction. Sept 21-23, 2001. Edinburgh, Scotland.
- Journal of Orthopaedic Science. 2002. 7: 199 – 20
- Romanes GJ (1981) Cunningham’s Textbook of Anatomy. Toronto: Oxford University Press.
- Kapandji IA (1974) The Physiology of the Joints, vol. 3. New York: Churchill Livingstone.
- Research Quarterly for Exercise and Sport. 1980. 51, 334–348
- European Journal of Applied Physiology. 1985. 54, 524–532
- Acta Orthop Scand. 1966. 37:177–190
- Acta Orthopaedica Scandinavica. 1968. 39:47-57
- Nordin M and Frankel V (1989) Basic Biomechanics of the Musculosceletal System. Malvern: Lea & Febiger.
- Crisco JJ, Panjabi MM (1990) Postural biomechanical stability and gross muscular architecture in the spine. In Multiple Muscle Systems: Biomechanics and Movement Organization (ed. Winters J, Woo S). New York: Springer.
- Journal of Orthopedic Research. 1991. 19:228-236
- McGill S 2002 Low Back Disorders. Evidence-Based Prevention and Rehabilitation. Human Kinetics, Champaign, IL
- J Appl Physiol. 1997; 83(3):753–760
- Arch Phys Med Rehab. 2001; 82(8):1081–1088
- Neurology and Urodynamics. 2001. 20:31-42
- Richardson C, Jull G, Hides J, Hodges P 1999 Therapeutic Exercise for Spinal Stabilisation: Scientific basis and practical techniques. Churchill Livingstone, Edinburgh
- 2004; 29(22):E515–E519
- Medicine & Science In Sports & Exercise. 1998. 30(2):301-310
- 1998; 23(18):1937–1945
- 1995; 20(2):192–198
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.











