Plantar fascia ruptures

Medial plantar heel pain is a common overuse injury in running based athletes or in those who stand on their feet for extended periods of time. The most common pathological conditions resulting in medial plantar heel pain include plantar fasciitis (arguably the most common of all heel pains, also called fasciosis/fasciopathy), fat pad contusions, calcaneal stress fracture, tarsal tunnel syndrome and nerve entrapments (such as Baxter’s nerve – see the article here on Baxter’s nerve injuries)(1).
One uncommon sequalae of long term heel pain can be acute or chronic plantar fascia rupture in athletes. Rupture of the plantar fascia can affect athletes who land and jump, or those who are exposed to high acceleration and deceleration forces (basketball, tennis, rugby, soccer, gymnastics). Frequently, plantar fascia symptoms have preceded the spontaneous rupture. These connective tissue ruptures are not as functionally limiting as other connective tissue ruptures (such as the Achilles tendon); however, they may cause some long-term issues for the athlete if left unmanaged.
Anatomy and biomechanics
The term plantar fascia and plantar aponeurosis are used interchangeably in the literature. The distinction between the two is for academic purposes only. However, research suggests that the connective tissue has features that make it a fascia-like more than aponeurosis-like. The plantar fascia is a broad and thick fibrous aponeurosis/fascia that helps to support the arch of the foot. It is comprised of three distinct heads(2):- A thick central component, which attaches to the medial tubercle of the calcaneus. This portion is the most likely to be involved in plantar fasciitis.
- A thinner medial component.
- A thinner lateral component.
Distally, it extends to the toes and divides into five digital bands that insert to the base of the periosteum of the proximal phalanx of each toe, and the short transverse metatarsal ligaments of the metatarsal heads. These five digital bands then divide into the metatarsophalangeal joints, forming the fibrous flexor sheaths on the plantar aspects of the toes. This also blends with the dermis(2)
In a seminal academic article in 1954, Hicks showed that the plantar fascia is tensioned during the latter stages of weight bearing, and as the metatarsophalangeal joints dorsiflex this applies a tractional force at its point of insertion on the calcaneum(2). As a result, the distance between the calcaneus to the metatarsal heads decreases and the arch will rise and become rigid. This mechanism he called the ‘windlass effect’ (see figure 1).
The ‘windlass effect’ plays an important role in dynamic function of the foot during walking and running. It elongates during stance phase of weight bearing, and then stores potential energy during this motion. During toe off, this ‘windlass mechanism’ locks the midfoot and provides a stable and rigid midfoot for toe off and propulsion. The stored potential energy is then released into kinetic energy and this aids propulsion and acceleration.
Figure 1: The windlass effect
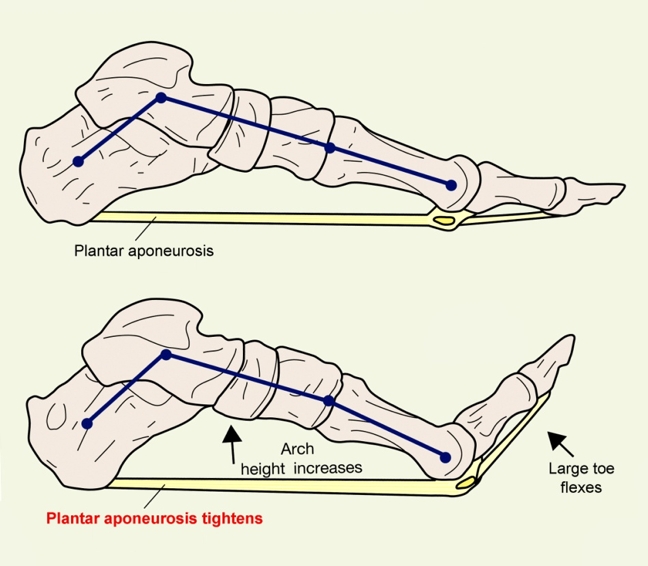
As the foot rolls forward on impact, the big toe flexes, which increases the foot arch height, stretching the plantar aponeurosis. As the toe straightens on push off, the arch lowers and the stored energy in the plantar aponeurosis can be released, increasing the push off power.
This ‘windlass’ concept requires that the plantar fascia remains quite rigid to draw the bones into a rigid and forefoot supinated position, and thus support bodyweight. A flexible and elastic plantar fascia would simply absorb too much energy and not create a windlass mechanism. This has been supported by a recent mathematical model that revealed that very large forces (outside the normal physiologic range) are required to produce even 1% compression and 1% shear in the plantar fascia(3). Therefore, to summarise the major anatomical features of the plantar fascia and the ‘windlass mechanism’:
- The plantar aponeurosis has a mechanically strong attachment at its distal end through the plantar pads of the metatarso-phalangeal joints to the proximal phalanges.
- When the toes are extended they pull the plantar pads and hence the aponeurosis forward around the heads of the metatarsals, like a cable being wound on to a windlass. The arch is caused to rise because the distance between the metatarsal heads and the calcaneum is thereby shortened.
- The toes are forced into an extended position in toe-standing and walking by the action of body weight. The arch is caused to rise by this ligamentous mechanism, without the direct action of any muscle.
Plantar fascia and the Achilles
In younger people, the plantar fascia has a unique connection to the Achilles tendon(4). This connection comprises a layer of periosteal fibres, which declines in thickness and elastic properties with aging(5). In an MRI study by Kim et al, it was found that the insertion of the Achilles tendon on magnetic resonance images (MRI) in older people had a more proximally inserted Achilles tendon than in younger people(6). From a morphological point of view, these results indicate that a connection between the Achilles tendon and the plantar fascia is more likely in younger people.Considering this anatomical connection between the Achilles and plantar fascia, many rehabilitation protocols recommend always considering the calf muscles in rehabilitation treatments for plantar fasciitis(7). This is supported by a three-dimensional model of the human foot and ankle by Cheung, which investigated the loading response of the plantar fascia in the standing foot with different magnitudes of Achilles tendon loading(8). It found that increasing tension on the Achilles tendon is coupled with an increasing strain on the plantar fascia.
Fascia or aponeurosis?
In a biochemical and histological study, Stecco et al used different stains to highlight the fibre arrangement of the plantar fascia(9). They found that the fibres were primarily arranged in a proximal to distal longitudinal direction, with fibres also in a vertical, transverse and oblique direction. This multilayer arrangement is more typical of a fascia and not an aponeurosis.These fibres were primarily type-1 collagen fibres; only in the loose connective tissue where the fibre bundles changed direction were type-3 collagen fibres found (see box 1). Furthermore, elastic fibres were only found in the loose connective tissue, adding further evidence that the plantar fascia is not elastic but has the appearance of a rigid tendon. Finally, it was found that the plantar fascia was heavily innervated with Pacini and Ruffini corpuscles. This suggests it has a proprioceptive and stability function in the foot – ie it may be able to perceive the intricate position of the foot and the state of contraction of the various intrinsic muscles of the foot.
| Collagen type | Main sites | Special Features |
|---|---|---|
| Type I | Bones, tendons, organ capsules, dentin | Most abundant, typical collagen fibre (64nm banding) |
| Type II | Hyaline cartilage, elastic cartilage | Very thin fibrils |
| Type III | Reticular fibres | Often associated with Type I |
| Type IV | Basal lamina associated with epithelial and endothelial cells | Amorphous (non-fibrous) |
| Type V | Basal lamina associated with muscle | Amorphous (non-fibrous) |
Plantar fascia ruptures
*Signs and Symptoms
Plantar fascia ruptures are not a common injury in athletes. If they do occur, they most commonly present as an acute lesion on chronic plantar fasciitis that has been previously treated with corticosteroid injections. It is argued that corticosteroid injections can lead to a weakening of the plantar fascia and this may evolve to an acute rupture over time(10-12). They may however also rupture in a weakened plantar fascia that has developing degeneration.
The clinical presentation of acute plantar fascia rupture differs from plantar fasciitis. The key features of a plantar fascia rupture are as follows:
- The athlete will feel a sudden sharp pain and popping sensation as the fascia ruptures.
- The pain of an acute rupture is located more distal to the insertion of the plantar fascia, whereas acute plantar fasciitis is painful on the calcaneal insertion.
- In the days after rupture, bruising and ecchymosis is commonly seen along the middle of the arch.
- The midfoot will be extremely tender to touch whereas in fasciitis the common spot of tenderness is the calcaneal insertion.
- The athlete will have trouble walking at all times, whereas in fasciitis it is the characteristic morning pain upon wakening.
Most often, clinical evaluation, activity of the patient and onset of pain will help the practitioner determine the extent of injury and determine fascia strain/rupture from fasciitis. It appears that rupture of the medial band is the most common variation of plantar fascia ruptures(13,14).
*Imaging
The most sensitive imaging modality is MRI, which is superior to other modalities in differentiating acute plantar fasciitis, and chronic plantar fasciitis from partial or acute plantar fascial rupture. MRI imaging will determine the exact location and extent (proportionate thickness and amount of oedema) of fascial rupture.
Here are a few summary points regarding MRI imaging for plantar fascia rupture(15, 16):
- The attachment of the plantar fascia is best demonstrated on coronal images.
- The entire course of the fascia is best seen on the sagittal images.
- Visualising of the medial fascial band is best seen in the sagittal and coronal views.
- The lateral band is best observed with oblique imaging, although sagittal and coronal images can also be used.
- In plantar fascial rupture, there is often a fusiform appearance of the fascia.
- There is also widespread abnormal high signal intensity infiltrating perifascial soft tissues consistent with local oedema that increases the size of the fascia(15).
*Treatment
Treating and athlete with an acute plantar fascia rupture can vary on extent of injury and the sport the athlete participates in. Historically, plantar fascia ruptures were managed conservatively with initial non-weight bearing and this was progressed as tolerated. Ice packs and anti-inflammatory agents (medications and electrotherapy) have also been recommended to settle the pain and swelling, followed by orthotics to passively support the arch of the foot. Currently, there are no comparative reports on conservative versus operative management for acute rupture, although it does appear that conservative management does work well even in elite athletes.
In a study conducted four decades ago, Leach et al reported on suspected partial ruptures in six long-distance runners who were treated conservatively (MRI and ultrasound imaging was not commonly used 40 years ago)(11). Only one patient required surgery (fascial release) for persistent swelling. The remaining runners all reported full recovery back to their original pre-injury activity with no deleterious effects, even in the one surgical patient.
In a more recent study, Saxena and Fullem reviewed 18 subjects (including six elite athletes) who had suffered plantar fascia ruptures(13). All were managed with a 2-3 week period of non-weight bearing in a cast/boot, followed by 2-3 weeks progressive weight-bearing with physiotherapy intervention. All 18 returned to their chosen sports without complications. The mean return time was 9.1 weeks albeit with a fair degree of variability.
Clinically, it makes sense to work on strengthening the small foot intrinsics such as the flexor digitorum brevis, flexor hallucis brevis, lumbricals and plantar interossei in the event of a plantar fascia rupture, as they will help give the arch some active support (in the presence of diminished support from an attenuated plantar fascia). This type of intrinsic strengthening can be performed with simple arch strengthening exercises such as towel scrunch exercises and the cup-drop exercise (see figures 2 and 3).
Figure 2: Towel scrunches




- Towel scrunches strengthen the muscles that support the arch of the foot.
- Place a towel on a tiled or wooden floor (carpet won’t work).
- Place the foot relaxed on the towel with the foot in line with the knee and hip. The toes should be pointing directly ahead.
- Initiate the movement by attempting to firstly lift the arch. Think about drawing the ball of the foot towards the heel. You will see the arch will lift.
- Next use all the toes to curl the towel under the foot.
- Relax the foot and start again.
- This exercise does not cause any soreness the next day, what will be felt is that the arch muscles will start to fatigue.
- The progression is seated, to standing on two legs and standing on one leg.
Figure 3: The cup drop exercise



- The cup dropis an interesting and novel way to integrate both intrinsic arch muscle function and extrinsic anti-pronator muscle function with hip stability muscles - in particular the gluteus medius and maximus. During weightbearing, the gluteus medus muscle prevents the hip from internally rotating and adducting, and this action works well with the arch muscles preventing excessive pronation.
- Place some small objects such as marbles about one foot in front of your body.
- Reach forward with the foot and pick up the marble with the toes. This action of clawing the marble with the toes will stimulate the arch muscles.
- Whilst holding the marble in the toes, circle the hip outwards to the side of the body and then behind the body and place the marble in a cup placed at 45 degrees to the hip.
- It is important that the foot stays turned outwards during the circle movement as this keeps the gluteus active.
Although it appears that most plantar fascia ruptures respond well to conservative care, the long-standing effect to the lower limb kinetic chain function can be profound if certain corrective measures are not employed. A conservatively managed plantar fascia will anatomically become longer as it scars and heals. The decrease in tension of the fascia and the negative effect on the windlass mechanism in stance and propulsion phases of gait will prolong pronation forces in the foot, flatten the longitudinal arch and increase pressures in the forefoot(17).
The biomechanical effect of this is that because the medial column is less stable, the athlete will naturally shift the load and force areas towards the lateral foot to maintain a degree of stability. This may manifest long term as lateral foot pain and lateral metatarsal stress fractures. This may also lead to ‘first ray’ compensations and deformities as the first ray (via the peroneus longus) will attempt to stabilise the medial column(18). Therefore, proper management of a conservatively treated plantar fascia rupture should involve a thorough podiatrist work up with custom made orthotics, to give the forefoot and midfoot reasonable passive stability.
References
- Brukner P and Khan K (2017) Clinical Sports Medicine (5thEdition). McGraw Hill. Australia
- Journal of Anatomy. 1954; 88: 25–30
- 108(8); 2008. 379-390
- Journal of Anatomy. 2008; 213, 718–724
- Foot Ankle Int. 1995. 16, 418–421
- J Foot Ankle Surg. 2011. 50, 41
- Foot Ankle Int.2000 Jan;21(1):18-25
- Clin Biomech (Bristol, Avon). 21(2):194-203
- Journal of Anatomy. 2013; 223, 665—676
- Eur J Sport Sci. 2017. 17(6): 765-793
- J Bone Joint Surg Am. 1978. 60 (4): 537-539
- Foot Ankle Int. 1994. 15(7): 376-381. 12
- Am J Sports Med.2004;32(3):662-5
- The Journal of Foot and Ankle Surgery. 1997. 36(2); 112-114
- 2000. 20: S181- S197
- The Foot and Ankle Online Journal. 2009. 2(5); 4
- Curr Rev Musculoskelet Med. 2009; 2:3–9
- Foot Ankle Spec. 2010, 3: 335
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









