Lateral epicondylitis: assessment and rehabilitation

Lateral epicondylitis (LE) - commonly referred to as tennis elbow - is the most frequently diagnosed condition affecting the elbow. Tennis players often experience elbow pain, with 50% of players reporting pain. Of these cases, 80% relate to LE(1). Archers or shooters may also present with pain relating to the lateral epicondyle and the extensor tendon(2). In addition, up to 17% of manual workers in industries requiring repetitive hand tasks commonly present with LE(1).
Lateral epicondylitis commonly affects people over 30 years of age and those pursuing activities requiring repetitive movements of the forearm. Pain may be aggravated by the gripping of small objects such as in racket sport-based movements, as well as painting and hammering. In 1936, Dr James Cyriax stated that the duration of symptoms for LE could typically last as long as six months and possibly up to two years. This is still true in the modern era; 50% of patients still present with LE related symptoms 12 months after presenting in clinical practice(1).
Anatomy and biomechanics
The primary structures involved in LE are the extensor carpi radialis brevis (ECRB), and less frequently, the extensor carpi radialis longus (ECRL)(2). These structures originate at the lateral epicondyle of the distal humerus, and attach via the extensor tendon (see figure 1). The muscle tendon junction of the ECRB is in the mid forearm (where the tendon courses in conjunction with the ECRL) beneath the extensor retinaculum, and inserts onto the lateral dorsal surface of the third metacarpal bone.The ECRB is primarily a wrist extensor but also abducts the hand at the wrist joint. The ECRB is under greatest strain when its fibres contract whilst in forearm pronation coupled with wrist flexion and ulnar deviation. This is the position replicated during an incorrect back hand stroke in tennis, which explains the popular label of ‘tennis elbow’.
Figure 1: Extensor mechanism of the lateral elbow

Efforts should be made to educate tennis players on techniques for correctly executing a backhand in tennis. It is often observed that a tennis player will use two hands to prevent overload to the wrist extensors. If a second hand isn’t used as support and the arm is straight (see figure 2), the loading on the extensor tendon when the ball impacts the racquet can be very high. An alternative is to execute the shot with a flexed elbow where possible, to reduce this impact loading.
Figure 2: Incorrect backhand technique in tennis

Not overreaching also allows for a stable platform through the legs and trunk muscles. Compare this to an overreached position, where there is little control of the trunk and legs, which leads to a greater load applied at the extensor tendon from potentially forced wrist flexion, at the point where the ball makes contact with the racquet. It is essential therefore to select an appropriately sized grip for the tennis player. This can be determined by the width of the fifth digit; in an optimally-sized tennis racquet grip, it should fit between the longest finger and the thenar eminence (see figure 3).
Figure 3: Selecting the correct tennis racquet grip size(3)

Examination and assessment
An assessment of a patient presenting with lateral elbow pain should include grip strength using a hand-held dynamometer – up to a loading where pain presents(1). This allows repeated measurements in comparison to the non-involved arm. Active, passive and resisted movements of the elbow, forearm and wrist must be performed - as well as the neurodynamic testing of the radial nerve to rule out spinal pathology(1). The special tests for testing medial and lateral ligament instability should also be included. It is useful to obtain an outcome measure; the patient rated ‘tennis evaluation scale’ is a useful condition-specific tool. It spans from 0 (no pain or disability) to 100 (worst pain or disability), and factors in both pain and function(1).In patients presenting with lateral elbow pain, it is possible for multiple pathologies to coexist. Researchers from Uppsala University, Sweden assessed the incidence of pain in the cervical and thoracic spine (C2 – T7) in those with and without lateral elbow pain(4). Thirty-one patients with lateral elbow pain and 31 healthy control persons participated in this study. The results showed that 70% of patients with lateral elbow pain had pain on palpation in the cervical or thoracic spines, which contrasted to 16% in the control group. Pain responses to the cervical and thoracic provocation tests were significantly higher in the lateral elbow pain group. The frequency of pain was also significantly greater on neurodynamic testing of the radial nerve in the lateral elbow pain group.
An abundance of special tests are available to assist with a diagnosis of LE. These include the Cozen, Maudsley and Mills tests (see table 1). Researchers from the Sri Ramachandra University in India, studied the diagnostic accuracy of these three tests when compared with musculoskeletal ultrasonography(2). Ultrasonography is effective diagnosing tendon related pain as it determines tendon thickness (a common feature in LE), and fluid content(2). Thirty patients aged between 30-45 years with a diagnosis of LE were recruited. Patients presenting with cervical radiculopathy, neurological disorders and fractures close to the lateral elbow were excluded from the study. Pain severity was measured during each of the three tests and correlated with the findings from the diagnostic ultrasound.
This study assessed specificity and sensitivity of the three tests in Table 1. Specificity determines the proportion of negatives that are correctly identified (for example if the test result for a highly specific test is positive you can be nearly certain that they actually have the condition). Sensitivity assesses the proportion of positives that are correctly recognised (for example if the test is highly sensitive and the test result is negative you can be nearly certain that they don’t have the condition).
Maudsley’s test had good sensitivity (88%) but poor specificity (0%). Cozens test had good sensitivity (84%) but poor specificity (0%). In comparison Mills test had an average sensitivity of 53% but excellent specificity of 100%. Of the 30 patients 14 tested positive for LE and 16 negative for LE on Mills test. Of the 14 patients who tested positive for LE on Mills test all 14 also had a positive correlation on ultrasound. Of the 16 patients who tested negatively on Mills test, four actually tested positive on ultrasound for LE.
Table 1: Three primary tests used in the examination of a patient with lateral elbow pain(2)

Cozen’s test: The patient should be placed in a sitting position with the elbow supported with the forearm pronated. The therapist places his/her thumb over lateral epicondyle in order to help stabilise the arm. The patient is instructed to make a fist with wrist in extension with the therapist passively moving the wrist into radial deviation whilst maintaining pronation throughout. The therapist applies resistance to the wrist in extension; pain felt over the lateral aspect of the elbow joint indicates a positive test for LE.

Maudsley test : The patient is seated with the elbow flexed to 90° and the forearm pronated. The patient is then asked to extend the middle finger against with the therapist applying resistance. Pain over the lateral aspect elbow joint indicates a positive test for LE.

Mills test: The subject is positioned in standing with the shoulder slightly abducted and the elbow flexed to 90°. The forearm is pronated and the wrist flexed so that the palm of the hand would face downwards. The therapist is positioned beside the patient’s affected side, with one hand grasping the upper arm for support. The forearm and wrist are maintained in pronation and flexion respectively whilst the elbow is extended slowly (as shown). Pain over the lateral aspect of the elbow joint indicates a positive test for LE.
Exercise therapy
A wide variety of treatment modalities exist for LE, and it is not uncommon for a patient to present in the physiotherapy clinic having already had one or more steroid injections. Before injection therapy is considered, the options of exercise and manual therapy, should be thoroughly explored. No one single specific protocol exists in the rehabilitation of LE - therefore an abundance of interventions are possible(5).A six-week randomised controlled trial (RCT) was carried out by researchers in Sweden, which compared the effects of eccentric forearm resistance exercise (provided by a bucket of water – see figures 4 and 5) with the use of a forearm resistance band(6). Forty-two participants with a diagnosis of LE were randomly allocated to either group. Eccentric exercise was performed daily using an appropriate weight to maintain a pain free range for two sets of 8-12 repetitions for the first week and then increasing to two cycles of the same routine in week two and then to three cycles of the same routine in week three and so on.
The results indicated that at the three-week intervention point, there were no differences in grip strength or wrist extensor strength observed between the eccentric or resistance band groups. By contrast, there was a significant difference at the six weeks follow up. The eccentric exercise group subjects experience a significant decrease in LE symptoms, with 56% reporting being pain free at the six-week intervention point. This was in comparison to the control group, where 79% of subjects still complained of symptoms of LE. This study suggests that daily eccentric loading exercises can reduce the symptoms of LE.
Figure 4: Eccentric exercise using a bucket with water (allowing for adjustable resistance)
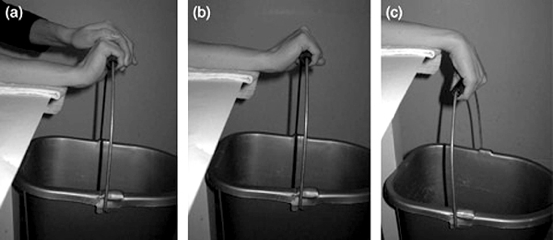
A - Subject lifting bucket with force from non-affected arm to avoid the concentric phase on the involved arm.
B - Starting position for eccentric contraction of affected forearm extensors.
C- Final position with the wrist in flexion.
Figure 5: Tyler Twist exercise for eccentric loading of the forearm wrist extensors
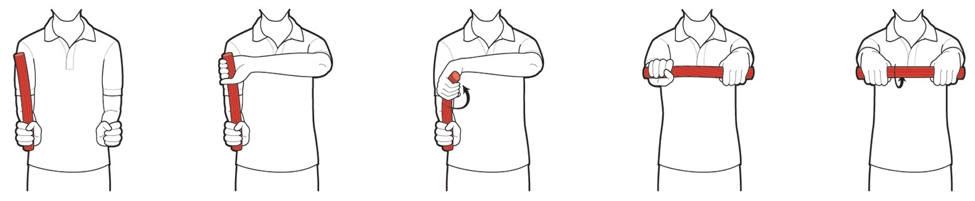
The Tyler twist is a functional movement completed daily, and is a progression of the exercise carried out in figure 4. It is performed as follows:
- The client holds a twist bar vertically with the affected arm.
- He/she reaches across and grabs the bar with the other hand, palm facing outward.
- Keep the injured arm still, the bar is twisted clockwise with the top hand.
- The twist is maintained while extending the arms and turning the bar horizontally.
- He/she slowly untwists the bar using ONLY the hand of the injured arm.
Orthosis
It is common practice to see people on the tennis courts with an orthotic brace on the upper forearm. But how effective are these devices? In one study, researchers surveyed the existing literature combining several RCTs(1). They found that there were minimal differences between braces. Compared to no treatment or taping techniques, the authors noted a marginal improvement in pain and function over a four to 12-week intervention period when using these devices. In addition, a brace may be as effective as injection therapy in relieving pain over a short-term period of two to six weeks(7).Exercise versus injection therapy
Injection therapy is a time-efficient method of obtaining quick results but there are risks involved in this form of treatment, and it is important to review the long-term follow up. Researchers from the University of Queensland studied the effectiveness of corticosteroid injection, multimodal physiotherapy or both, in patients with LE(8). One hundred and sixty-five participants with LE were randomly divided into either a corticosteroid injection group (43 subjects), placebo injection group (41 subjects), corticosteroid injection plus physiotherapy group (40 subjects) or placebo injection plus physiotherapy group (41 subjects). The physiotherapy consisted of mobilisations of the elbow joint, as well as progressive concentric and eccentric resisted exercises of the wrist extensors. Follow ups were performed at four, eight and 26 weeks.The key finding of this study was that at the four week follow up, there was a significant effect noted with the patients receiving the placebo injection plus physiotherapy obtaining a greater complete recovery (39%) compared those receiving the steroid injection and no physiotherapy (10%). There was no beneficial effect to having a steroid injection alone – in fact, there was a greater effect on pain by using a physiotherapy treatment alone with a placebo injection.
Manual therapy
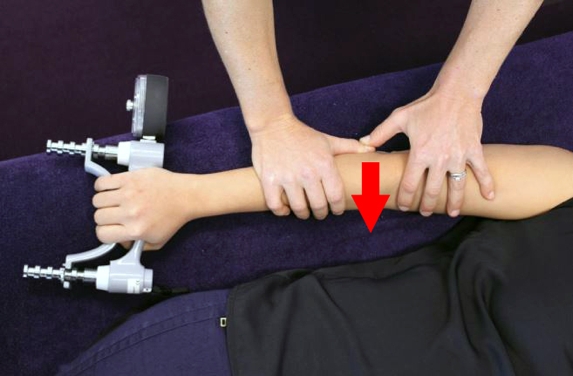
Manual therapy in the form of friction massage and joint mobilisations to the lateral elbow are proposed as useful treatment tools. Clinicians from the University of Queensland described the use of mobilisation with movement, whereby a postero-anterior glide of the radial head was performed (see figure 6)(9). The mobilisation was carried out at the same time as the painful action of intermittent gripping, which provides useful feedback. This technique can be repeated for 30 seconds over three to six sets based on the patient’s tolerance. However, there is a paucity of research investigating the effects of massage alone and therefore manual therapy may be best used in conjunction with eccentric exercise.Figure 6: Postero-anterior glide of the radial head
Summary
Lateral epicondylitis is a common condition amongst manual workers, and in athletes participating in racket and throwing sports. There are a variety of factors that predispose its onset. The Mills test for LE has a higher specificity and sensitivity score for diagnosing LE compared to other measures. Eccentric exercise for a six-week period has been shown to be effective in reducing the symptoms of LE. The physiotherapy protocols should be used intensively with daily intervention exercises before the use of injection therapy. The effectiveness of injection therapy over the long term does not seem to be as effective as physiotherapy interventions, which are less invasive.References
- J Physiother, 2015, 61, 174 – 181
- Int J Physiother Res, 2014, 2, 6, 815-2
- Sports Heal, 2013, Apr, 5, 2, 186 – 194
- Musculo Sci & Prac, 2008, Aug, 13, 4, 295 – 299
- The Sci World J, 2011, Nov, 2012, 1 – 8
- Scand J Med Sci Sports, 2012, 22, 797 – 803
- JAMA, 2013, Feb, 309, 5, 461 – 469
- J of Ortho & Sports Phys Thera, 45, 11, 938 – 949
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Injury Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









