You are viewing 1 of your 1 free articles
Getting straight to the point on triceps tendon injuries

Tendinopathies of the triceps tendon, and the potential serious sequalae of partial and complete ruptures, are a relatively rare but debilitating condition that can affect power athletes(1). For the power athlete participating in a ‘push’ based sport such as powerlifting, contact football, and martial arts/combat sports, triceps tendon pathology can cause significant symptoms and be functionally limiting(2-4).
The more common tendon injuries include the lateral and medial epicondyle tendons (extensor origin and flexor origin) and the distal bicep tendon(5). It has been estimated (using magnetic resonance imaging [MRI]) that only 3.8% of tendinopathies affect the triceps tendon(6). Along the triceps tendon injury continuum, partial tears are the most common triceps injury comprising around 23% of the distal triceps tendon injuries.
As the average age of those injured is around 46 years, this suggests that developing tendon degeneration is a necessary precursor to partial or complete rupture(6). The serious end-stage pathology is a tendon rupture; however, this has been estimated to be extremely rare (in less than 1% of serious tendon injuries to the upper limb)(1).
It is more common for serious injuries such as tendon rupture to affect males between the ages of 40-50 at a ratio of 11:1 ratio of males to females(6,10,11). The incidence of chronic triceps tendinopathy is unknown; many cases of triceps tendon pain may go unreported as often, gym goers simply modify the choice of exercises to avoid tendon pain.
Anatomy
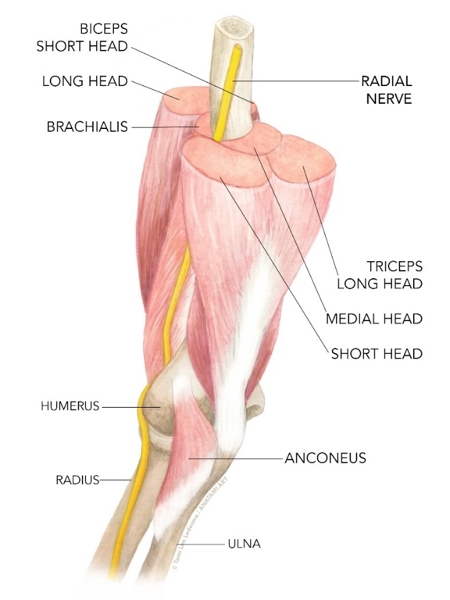
The primary function of the triceps is to extend the elbow, and the long head of the triceps can also assist in shoulder extension movements. The exact anatomy of the distal triceps insertion may therefore be important for the surgeon to understand when repairing the distal triceps tendon.The triceps brachii is composed of three muscle bellies (see figures 1 and 2)(7):
- The long head arises off the infraglenoid tubercle of the scapula. As this muscle crosses two joints, it is bi-articular and is influenced by the shoulder flexion angle.
- The medial head originates off the posterior aspect of the humerus distal to the spiral groove.
- The lateral head originates off the lateral intermuscular septum and the posterolateral aspect of the humerus above the spiral groove.
Figure 1: Anatomy of the triceps muscle
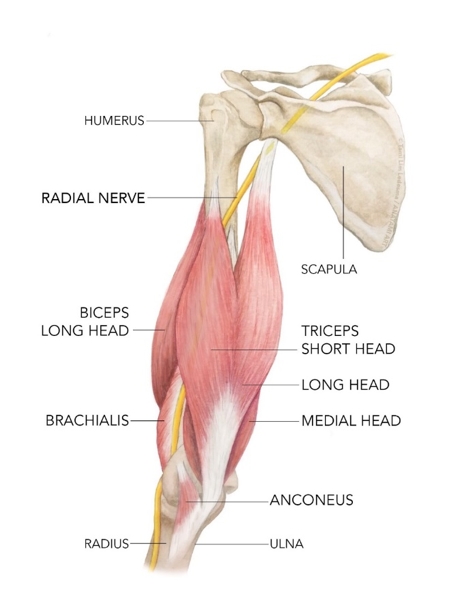
The exact anatomy of the insertion of the triceps remains controversial. Agreement tends to exist as to the exact anatomy of the superficial portion of the insertion. This tendon is believed to be made up of the lateral and long heads that converge, and then insert medially straight into the medial aspect of the olecranon. Laterally, the fibres insert at an angle and then continue to blend with the superficial fascia of anconeus (sometimes referred to as the lateral expansion).
The anatomy of the medial head tendon of the triceps is more contentious:
- Madsen et al believe the medial head to have a separate, deep insertion from the central tendon (from cadaveric studies(8)).
- In another cadaveric study, Keener et al described a thickening of the medial aspect of the tendon that was not distinct from the central tendon with fibres from the medial and long heads of triceps(9). The insertion was not separate from the central tendon.
- In another dissection study, it was found that approximately half of the specimens had a discrete tendinous portion of the medial triceps that was deep to the long and lateral heads of the triceps. The long head and lateral head form a tendon that is superficial to this discrete medial portion(10). In the other half of the specimens, a common combined tendon insertion was found; however these still had medial fibres that were deep to the long and lateral head fibres.
Figure 2: Anatomy of the triceps muscle (showing the position of the three heads)
Injury types
*Tendinopathy
This most commonly occurs at the tendon attachment to the bone at the olecranon(12), but can occur within the tendon substance or at the musculotendinous junction. In athletes, the classic systemic risk factors that weaken tendons are not as common as in the general population. However, these may include metabolic conditions and endocrine disorders such as diabetes mellitus and hypoparathyroidism(13-15). What may be more relevant for the athlete are the local factors that may weaken or traumatise the tendon, such as corticosteroid injections(16), anabolic steroids(16), overtraining, and olecranon bursitis (which has also been implicated in tendon rupture)(12).
Tendon pain in gym athletes is typically felt during exercises such as lying triceps extensions and overhead triceps extensions. However, pain is usually manageable if the lifter performs triceps pressdowns and dips. It is theorised that positions of increasing shoulder flexion place the long head of the triceps under greater stretch. This greater stretch and greater tensile load - coupled with the compressive load of the tendon pressing against the olecranon - may be enough to precipitate a tendinopathy.
*Acute tears
Acute tears of the triceps tendon may occur in a number of ways:
- A fall on an outstretched hand when a sudden deceleration stress is put on a contracted triceps muscle, such as a breaking a fall with an extended elbow. This would be common in a football player or martial artist.
- Strong triceps contraction during gym exercises such as bench press.
- Hitting a fixed resistance with the posterior elbow such as landing directly on the point of the elbow(10,17-20).
The most common sport associated with tendon tears is weightlifting(6,10,16,18,21-23), which has also often been associated with a history of steroid use(6,16,22).
*The ‘snapping triceps’ tendon
This dynamic phenomenon tends to occur in younger athletes (average age of 32 years) and with a slightly reduced male to female ratio of 6.5:1(24-27). It is characterised by a snapping sensation during both flexion and extension, with both active and passive movement of the elbow228).
This phenomenon is caused by a ‘dislocating’ triceps tendon either on the medial or lateral side of the elbow. Medial snapping is more common, and it may be painless or cause snapping with elbow pain and ulnar nerve neuropathy on the medial side(28, 29). It is common to have concurrent snapping of the tendon with dislocation of the ulnar nerve(28). It has been postulated that a snapping ulna nerve and snapping triceps could be differentiated by the angle at which the snapping occurs. The ulna nerve is thought to snap at 70-90 degrees of flexion, whereas the triceps is thought to snap at around 115 degrees of flexion(28).
A number of causes of medial snapping tendon have been proposed:
- A medial vector placed on the tendon with the elbow in a valgus position(30)or certain muscle activation patterns(27). This medial vector is a function of the T angle, where the T angle is the angle between the subtended line of pull of triceps (humeral shaft with extended elbow) and the longitudinal line of proximal ulna(27).
- A complication of displaced supracondylar fractures(31,32).
- Inherited as an accessory medial triceps or abnormal insertion(28).
- Hypertrophy of the medial triceps in athletes(28,31).
- Associated with hypermobility of the ulna nerve(29).
Signs and symptoms
Triceps tendinopathy is a characterised as a chronic condition resulting from overuse and repetitive heavy lifting. Swelling and palpable tenderness of the triceps tendon may be present on examination. The provocative sign will be resisted extension in positions of stretch (such as lying triceps extension), but strength is usually maintained. Tenderness to palpation occurs at the triceps insertion on the olecranon. In the setting of chronic repetitive injury, plain radiographs may reveal a traction osteophyte on the olecranon.Along the triceps injury continuum, a chronic tendinopathy may also then suffer strains and tears. Patients with spontaneous acute tears of the entire tendon typically present with ecchymosis, pain, swelling, extension lag and a decreased active range of motion at the elbow, while a palpable defect is commonly found and present in up to 80% of patients(19,22,28,33). Similar to Achilles tendon injuries, pain may often be absent prior to rupture of the tendon.
Partial tears may be confusing and not be as easy to diagnose initially. They may be easily missed as patients may lack power in elbow extension, while retaining a good range of active motion(10,34-36). Strength testing will show weakness of elbow extension. However, it is important to note that the ability of a patient to extend his or her elbow does not exclude triceps rupture, because elbow extension can be preserved in cases of partial tears though the lateral expansion of the triceps fascia. Furthermore, weakness in extension with the elbow flexed greater than 90° may be diagnostic of a partial extensor mechanism disruption (specifically, medial head triceps).
A complete inability to extend the elbow against gravity may represent a more significant injury to the triceps mechanism. Viegas has described a modification of the Thompson test (used to detect Achilles tendon ruptures) in which squeezing the triceps muscle belly does not produce expected elbow extension(37).
Imaging
It is common for disruption injuries of the triceps tendon to be complete avulsions off the olecranon; this is found intra-operatively in 33-73% of patients who suffer tendon tears. These correlate well to imaging findings of complete tears on X-ray and MRI. With acute tendon tears, a bony fleck proximal to the olecranon on radiographs is commonly identified(20-22,33), which is strongly suggestive of a triceps avulsion injury. This ‘bony fleck’ sign may also be demonstrated on ultrasound (see figure 3 below)(38,39).Figure 3: The ‘bony fleck’ sign
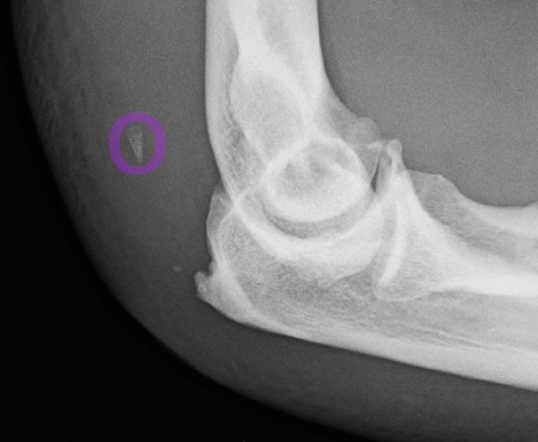
Bony fleck is shown circled.
The remainder of patients who don’t have complete avulsion injuries off the olecranon will have a rupture at the bone tendon junction(20,34). These triceps ruptures can be missed on X-ray, as the classic ‘bony fleck’ sign will not be present(20). Both ultrasound (US) and MRI have been used to diagnose complete tears and partial tears that do not involve the olecranon attachment(18,20,21,38). US has been reported to be as accurate as MRI for both complete and partial ruptures, including identifying the location of partial rupture(39).
The superficial location of the triceps tendon does however allow easy evaluation using ultrasonography compared to imaging other hidden tendons such as the distal biceps tendon. Ultrasound is performed with the elbow in flexion, and shows reduced echogenicity and occasional calcification in tendinopathy. Partial tears of the superficial or deep insertion of the triceps can also be readily seen(39).
MRI is used to visualise tendinopathy, and these scans may demonstrate an abnormal signal intensity on fluid sensitive sequences consistent with all forms of tendinopathy. The insertions of the superficial and deep portions of the tendon are also easily evaluated. In terms of diagnosing the snapping triceps tendon, US, MRI, computer tomography (CT) and sonoelastography have all been used for diagnosis(24-26,40). Ultrasound is the imaging modality of choice for some, as it can be used as a dynamically to differentiate between a snapping medial triceps and an ulnar nerve that is subluxing(24).
Injury management
*Managing tendinopathy
The knowledge in the management of triceps tendinopathy is not well developed or understood compared with the other common tendinopathies such as achilles, patella, upper hamstring, gluteals and wrist extensor tendons. The clinician can only extrapolate the ideas used in the management of these common tendinopathies and apply the principles to the triceps tendon. These basic principles are as follows(41):
- When reactive or ‘reactive on degenerative’ (when the tendon is angry), high load isometrics can be used to reduce pain via corticospinal inhibition. This is easily done using a single arm triceps pressdown hold in a mid-position (approximately 45 degrees elbow flexion). This should be done as heavy as possible so that:
- 45 seconds is sustainable without shaking.
- Pain levels are no more than 3/10 on the Visual Analogue Scale (VAS).
- Five sets of x 45 seconds with a 2-minute recovery can be tolerated.
- Weight can be progressed for isometrics, or the sufferer can progress onto heavy isotonics (see below).
- Heavy isotonics used when the pain is under control. This needs to be performed initially away from positions of high tendon compression (such as overhead triceps extensions or lying triceps extensions). The exercises most likely to be useful here are simple rope triceps pressdowns. These can be performed in the traditional four sets of 6 repetitions.
- Heavy eccentric loads such as single arm triceps pressdowns using two hands to push the weight down and using only one on the eccentric. Again, this needs to be in high volume, such as three sets of 15 repetitions.
- High tensile forces that store energy such as clap push ups are used for athletes who need high reactive strength and power in elbow extension.
*Managing tendon tears
Surgical repair is often recommended for complete tears or partial tears with significant weakness of elbow extension. Small partial tears can be successfully managed non-operatively. Even in patients with high functional demands (such as contact athletes), good results with non-operative treatment have been reported for the treatment of partial tears.
Patients are usually braced in a position of slight flexion (30 degrees) for approximately four weeks(7), and heavy lifting/pushing/resisted extension are avoided for up to 12 weeks(40). Adjunct treatments such as platelet rich plasma (PRP) injection have also been successfully used for the treatment of partial tears(18,42). Cheatham et al reported the results of a single patient treated with PRP with resolution of pain and return to gym four months after a PRP and physiotherapy regime(42).
For an acute tear of more than 50% shown on MRI together with significant loss of triceps power (power less than 60% of that pre-injury), operative repair of the torn tendon is recommended(43). Surgical repair is usually successful with minimum morbidity.
The management of chronic tendon ruptures is a challenge. For chronic ruptures with significant tendon retraction, reconstruction with a graft may be required. A number of grafts have been used to augment a primary repair such as achilles allograft (44,45), semitendinous tendon(33), aconeus(33), latisimus dorsi(33), plantaris(33)and palmaris longus(33).
In cases of acute triceps avulsion, timely surgical repair is advocated. Cases of incomplete tears where conservative measures have failed should also be treated operatively. Surgical technique involves primary repair of the avulsed triceps tendon using a Krakow suture pattern to the olecranon via bone tunnels(33). In general, surgical repair yields good results and return to activity.
The largest case series report to date from the Mayo Clinic utilised an Achilles tendon allograft in three cases of triceps tendon rupture or an anconeus muscle flap in four cases(44). From these seven cases, one rotation flap failed six months after operation. The remaining six patients had slight or no pain, restored functional range of movement and only slightly decreased extension power at 33 months follow up.
A few studies have attempted to evaluate the biomechanical properties of repaired triceps tendons. In an intact triceps tendon, the peak load to failure is at an average of 1714 Newtons(46). Direct repairs and augmented repairs fail at lower forces of 317 and 593 Newtons respectively. Different type of techniques such as trans-osseous cruciate sutures and bone tunnel and knotless suture techniques have also been studied for respective failure rates(7,33,46,47).
*Managing the ‘snapping tricep’ tendon
Initial conservative treatment can be attempted by avoiding the provoking activity for 3-6 months(40). Surgery can be tried if conservative treatment fails and this includes resection of the triceps edge, transposition of the tendon, transposing an associated ulnar nerve and correction of cubitus varus(40,48). Transposition involves transferring the medial third of the tendon to the lateral position(36,49).
Summary
Triceps tendon problems such as degenerative tendinopathy and partial/full tears are an uncommon and unusual injury in the athlete. If they do occur, they most likely occur due to direct contact onto the triceps tendon or falling and breaking he fall with an outstretched arm, when the triceps contracts strongly to break the fall. This injury is more common in ‘push’ based sports and contact athletes such as weightlifting, rugby/NFL and martial arts. Management of tendinopathies follows the same guidelines as other more common tendinopathies. Small partial tears can be managed conservatively whereas bigger partial tears and full thickness tears will require surgical reconstruction.References
- 1959;45(3):406-414
- Am J Sports Med. 1987;15(3):285-289.
- Am J Sports Med. 1987;15(5):514-516.
- Am J Sports Med. 2004;32(2):431-434.
- Clin Orthop Relat Res 2002; 40: 275-283.
- Skeletal Radiol 2011; 40: 587-594.
- Am J Sports Med 2010; 38: 1025-1033.
- Am J Sports Med 2006;34:1839–43.
- J Shoulder Elbow Surg 2010; 19:399–405
- Arthroscopy 2009; 25: 983-988.
- Orthop J Sports Med 2015; 3:
- J Shoulder Elbow Surg 2006; 15: 130-134.
- Ugeskr Laeger. 1982;144(37):2723.
- J Hand Surg Am. 1997;22(2):341-343.
- Acta Orthop Scand. 1987;58(4):434-435.
- J Shoulder Elbow Surg 1998; 7: 151-153
- Open Orthop J 2015; 9: 536-541.
- Orthopedics 2013; 36: 110-116.
- Arthroscopy 2012; 28: 1058-1063.
- Arch Orthop Trauma Surg 2011; 131: 1413-1417.
- J Orthop Case Rep 2015; 5: 58-61.
- Int J Sports Med 2000; 21: 308-310.
- J Orthop Sports Phys Ther 2013; 43: 848.
- Am J Phys Med Rehabil 2016; 95: e113-e114
- Pol J Radiol 2014; 79: 467-471.
- Radiographics 2014; 34: 1145-1162.
- Arch Phys Med Rehabil 2007; 88: 239-242.
- Tech Hand Up Extrem Surg 2002; 6: 91-97.
- J Bone Joint Surg Am 1998; 80: 239-247.
- J Shoulder Elbow Surg 2001; 10: 561-567.
- J Hand Surg Am 1999; 24: 381-385.
- J Shoulder Elbow Surg 2016; 25: e208-e21.
- J Bone Joint Surg Am 2003; 85-A: 1961-1967
- Arthroscopy 2014; 30: 785-789.
- Orthop Traumatol Surg Res 2012; 98: 242-246.
- Tech Hand Up Extrem Surg 2015; 19: 73-80
- Orthop Rev. 1990;19(6):533-536.
- J Ultrasound Med 2011; 30: 1351-1356.
- Eur J Radiol 2012; 81: 1207-1210.
- Tech Hand Up Extrem Surg 2002; 6: 91-97.
- Br J Sports Med.2015 Oct;49(19):1277-83
- Int J Sports Phys Ther 2013; 8: 290-299.
- Orthop Clin North Am, 1999; 30:95.
- J Bone Joint Surg Br 2002; 84: 1116-1120
- Arch Trauma Res 2016; 5: e32221 [PMID: 27148500 DOI: 10.5812/atr.32221]
- J Shoulder Elbow Surg 2011; 20: 213-218.
- Arthrosc Tech 2014; 3: e621-e626.
- J Hand Surg Am 1999; 24: 381-385.
- J Shoulder Elbow Surg 2016; 25: e208-e21.
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.









