You are viewing 1 of your 1 free articles
Case in point: Second metatarsal stress fracture - Part I
In the first part of a two-part article, Chris Mallac presents a case study of an elite footballer who suffered a proximal 2ndmetatarsal fracture and a 3rdmetatarsal stress reaction. In this issue, Chris discusses the causative factors in the pathogenesis of metatarsal stress fractures and how they are diagnosed.
Stress fractures of the metatarsals are a common overuse injury in athletes and dancers, and are only second to tibial stress fractures in terms of incidence(1). Stress fractures of the metatarsals are also common in military recruits and in long-distance runners and team sport athletes who cover large mileages in training and competition.
It has been reported that 10%(2)to 20%(3)of stress fractures in athletes, and 23%(4)of stress fractures in military recruits are located in the metatarsals. In terms of location, it is more common for the 2ndand 3rdmetatarsals to suffer stress reactions and fractures in the shaft and the non-proximal end of the bone. Indeed, the second and third metatarsal account for 80–90% of all metatarsal fractures(1,5,6). By contrast, proximal fractures in the heads of the metatarsals are not common.
Case study
A 21 year-old elite football player who plays as an attacking midfielder presented with acute onset, right-midfoot pain sustained in a training session. He described a sudden clicking sensation on the dorsum of the midfoot over the 2ndand 3rdmetatarsals. The injury was caused by a sudden change in direction. He was able to continue training for ten more minutes; however he noticed the pain in the foot was increasing. He denied any previous sensations of midfoot pain leading up to this injury, and had spent the previous 11 weeks of pre-season training completely injury free. His rehabilitation followed the 3-phase process.
Upon examination, the footballer was tender upon palpating the dorsum of the foot over the heads of the 2ndand 3rdmetatarsals. Pain was reproduced with walking on the toes and was also reproduced by squeezing the metatarsal heads together. The ‘piano key’ sign (grasping each toe individually and moving them in a plantar and dorsal direction) was pain free.
Based on these findings, it was suspected he had suffered either a subtle Lisfrancs injury or had injured the heads of the metatarsal’s, so an X-ray and MRI scan was requested to investigate further. The X-ray report was unremarkable. The MRI report however described bone oedema in the head of the 2ndmetatarsal and shaft of the 3rdmetatarsal, with a small fracture line evident in the head of the 2ndmetatarsal (see figure 1 below). No injury to the Lisfrancs ligament was reported.
Based on these findings the footballer was immobilised in a moon boot and instructed to mobilise in a non-weight bearing manner for an initial three weeks. He was then reviewed at three weeks and instructed to commence graduated rehabilitation (this will be discussed at length in part II).
Figure 1: MRI of the foot showing a small fracture line in the head of the 2ndmetatarsal

Causative factors
Using the B.E.E.T.R.O.O.T. acronym to identify the potential causative factors, a few elements were present that may have contributed to this stress fracture developing:
- B – Biomechanics. This player had previously suffered a talar dome fracture on the right ankle, and as a result, had lost some dorsiflexion. His standard lunge test measures (knee to wall) were 11cm on the left and 8cm on the right. He also demonstrated bilateral overpronation of the feet and a significantly longer 2ndmetatarsal compared to the 1st metatarsal.
- E-Environment. The outdoor surfaces this player had been training on in the previous 11 weeks had been extremely firm due to a dry spell. The ground firmness would have certainly contributed to the development of a stress injury.
- E-Equipment. This player had in the off-season, changed his football boot sponsor, and as a result had been training in a different football boot. He admitted that they felt like they compressed the forefoot more than his previous boots. This may have placed extra compressive forces on the metatarsal heads.
- T-Training. His acute and chronic workloads, high intensity work and change of direction aspects of training had been monitored using GPS and tracked by a sports scientist. This was to ensure he kept within the optimal 0.8-1.3 range of the ‘Acute to Chronic Work Ratio’ (ACWR)(7). This is presented in the table 1 and graph 1. The major variables important for a stress fracture would be a spike in volume and/or change of direction. It can be seen from the table and graph that he had no major spikes in these variables over the prior 11 weeks. Upon further questioning, he did disclose that he had a much greater consistency in training and playing (pre-season friendlies) volume compared to the previous season. If we looked over a larger six month period, we would argue that the last 11 weeks had been a significant jump on the previous season’s volume.
- R-Recovery. Although his ACWR fell within acceptable limits, the training program used in the pre-season had the players on their feet five consecutive days a week, without days off in between. They would play trial matches on the last day of the weekly training cycle, have two days off and then start the next cycle. It could be argued that in a younger athlete, these consecutive days may not allow time for bone adaptation (see table 1).
- O-Older. His age may have been a factor in this case as a 21 year old is still considered to not yet be skeletally mature.
- O-Overreaching. He did not have any external variables that may have acted as a catabolic stress factors (work, relationships, study etc).
- T-Threats.He had no known medical threats such as metabolic conditions, medications or diet issues that would have contributed to this problem.
Table 1: Acute to Chronic Work Ratio
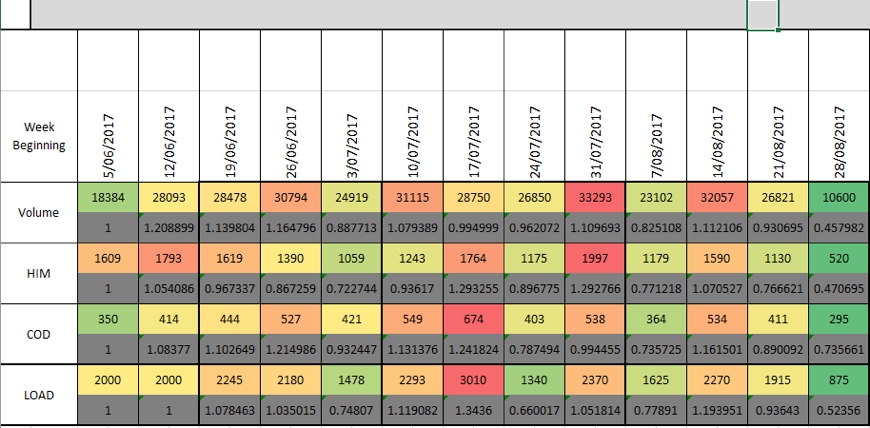
Weekly volume (m); HIM (high intensity metres); COD (change of direction); load (RPE x minutes)
The grey boxes show the ACWR (ratio) each week for each variable. The final column depicts the week he injured his metatarsal (3rdsession of the week).
Graph 1: ACWR shown as a bar graph
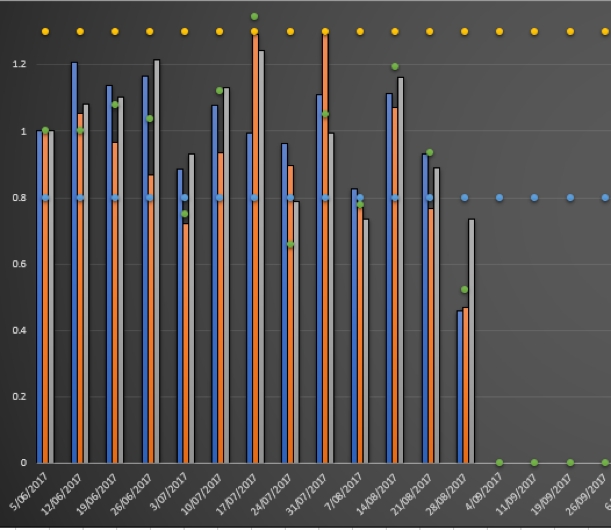
Blue bar is volume, orange bar is HIM and the grey bar is COD. Each bar should ideally fall in between the blue (0.8) and orange (1.3) dotted lines.
Anatomical and biomechanical considerations
Micheli was the first to write about stress fractures at the base of the second metatarsal in ballerinas in 1985(8), and this was expanded in 1996 by O’Malley who published the largest series on 64 fractures treated nonoperatively(9). In this unique population (dancers), the extreme plantar flexion of the foot and ankle for en-pointe position and the unique locking configuration of the second metatarsal and cuneiforms have been proposed as causes of this injury(10,11).
The metatarsal heads have unique anatomical features, which may predispose them to stress fractures. The second through to the fourth metatarsals have ligaments that anchor the heads of the metatarsals, and this protects them against fracture displacement. However, it also increases the forces acting across the plantar surface during weight bearing activities(12). The fixed bases and proximal hinged metatarsophalangeal joints create a bending moment at the proximal diaphysis during the stance phase of gait, and this may place excessive force across the metatarsals(13,14).
Although the second and third and metatarsals encounter the greatest peak pressures in weight bearing, they are also the weakest cross-sectionally(15). This is compounded by kinematic factors such as muscle fatigue(16), which decreases dissipation forces and increases stress on the metatarsals, thereby contributing to stress fractures(16,17), and the higher bending forces on the second metatarsal during running(13).
It has been suggested that 95% of fractures of the second metatarsal occur at the non-proximal aspect. Fractures at the head of the metatarsal (proximal end) are not as common. The recovery time of a proximal fracture is usually prolonged, delayed and non-union, often requiring surgical fixation(18-20). Proximal fractures are considered to be high-risk fractures compared with non-proximal fracture.
Risk factors associated with proximal stress fracture
Athletes with proximal stress fractures are more likely to have associated risk factors (reasons given where relevant)(21,22):
- Populations with mineral-deficient conditions such as rickets or osteomalacia may have bones with reduced mass/density, which are less able to withstand normal forces;
- Normally strong bones may be weakened by cysts or surgical or medical procedures, such as screw fixation, tendon transfer, joint arthroplasty, bunionectomy, or radiation treatment(23);
- The unique nutritional demands of women place them at a higher risk for insufficiency stress fractures than men. One explanation for this difference may be the female athlete’s susceptibility to the female athlete triad of eating disorders, amenorrhea and osteoporosis;
- Increased pronation is common among athletes with stress fractures of the lower extremity(24);
- Rigid cavus feet are a common predisposing factor to tarsal and femoral stress fractures(25);
- Hard surfaces;
- Inappropriate shoes or change in footwear;
- Increase in the intensity or type of exercise;
- Change in playing surfaces;
- Achilles tightness;
- To have size differences in length of first compared with second metatarsal;
- Participation in sport with a poor or reduced low levels of training.
A shorter first metatarsal compared with the second metatarsal (Morton’s toe) has been suggested to increase the risk of a second metatarsal stress fracture(26). A short first metatarsal produces abnormal overloading stress along the full second metatarsal length. In association with poor bone quality, a second metatarsal stress fracture may therefore occur at the weakest (proximal) location. The average length of the first metatarsal compared with the second metatarsal in patients with proximal stress fractures has been measured at approximately 73-82% of the length(21,22,26).
Pathogenesis
When a bone is loaded, the response of the bone is to remodel against the stressors imposed. The accepted wisdom has been that if the bone stress is too great then remodelling may not occur and periostitis, stress reactions and ultimately cortical stress fracture may develop(25). Stress fractures fall under two general classifications(23):
- Fatigue– abnormal stress loading to a normally elastic bone (more common in physically active populations).
- Insufficiency– normal stress to a bone that is mineral deficient or abnormally inelastic (most prevalent in nutrient-deficient and older populations).
With regards to fatigue fractures, the abnormal forces that cause a deterioration of healthy bone may result from:
- Increased training intensity;
- Hard surfaces;
- Worn/inappropriate shoes;
- Poor anatomical alignment of the feet.
It has been argued however, that to achieve the level of bone loading that can lead to stress fractures is not easy. It has been estimated that, at normal physiologic levels of strain, it would require 108 cycles of loading to produce failure of a weight-bearing bone such as the tibia(27). This is not easily achieved, and stress fractures commonly occur soon relatively quickly after the onset of a stressful activity(28). The rapid onset of symptoms and bone remodelling consistent with stress fracture suggests therefore that mechanical stress cannot be the only cause.
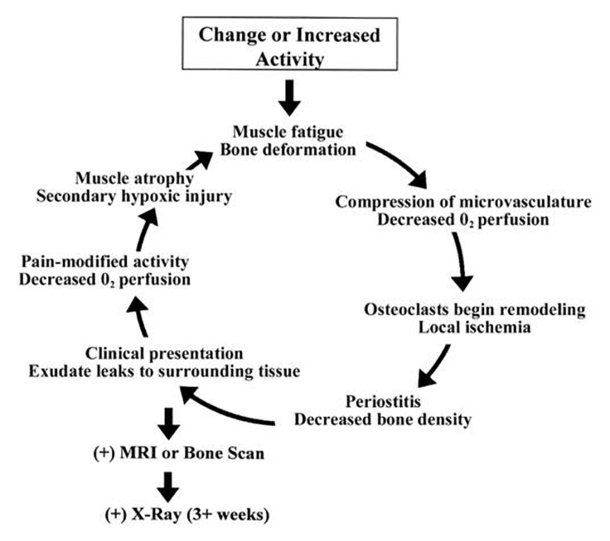
An alternative explanation for the development of a stress fracture is that a temporary oxygen debt occurs after perfusion and reperfusion of the bone after a repetitive load (see figure 2)(29). When high loads are imposed on the bone, the blood flow in the bone may be temporarily cut off, and this leads to a brief ischemia in the cells that would normally be perfused by the medullary vessels that are compressed(30,31). If blood flow and oxygen are restricted, then osteocytes (that breakdown bone) are channelled into the bone, and this leads to a weakened the bone that cannot withstand stress(32).
The local ischemia caused by poor blood flow appears to signal the beginning of osteoclast remodelling, decreased bone density, and periostitis. It is at this point that clinical signs of a stress fracture may be evident. Exudate from damaged blood vessels reduces oxygen perfusion to surrounding tissue and results in secondary hypoxic injury to surrounding bone cells(22).
Figure 2: Flow chart showing suggested ischemia-related mechanism for stress fracture(22)
Signs and symptoms
Athletes with 2ndmetatarsal stress fracture typically present with forefoot pain upon weight-bearing, inability to toe walk, focal swelling, and point tenderness. A history of change in terrain, training regime, and/or recent trauma is standard. Delayed diagnosis is relatively common given that the symptoms of stress fractures are fairly non-specific and do not lead to definitive disability(9). Importantly, stress fractures frequently occur in a cohort that is mostly reluctant to take time out of training until an injury becomes more actively disabling.
Imaging
It has been estimated that one-third of stress fractures may be missed on initial radiographs(9). Radiographs may be normal for the first 2–3 weeks after stress fracture development(33). It has been suggested that an MRI is necessary to differentiate a stress fracture from synovitis of the Lisfranc joint(34). Computer tomography (CT) may also play a part when identifying the exact location of the stress fracture and for assessment of healing and diagnosing non-union(35).
Summary
Stress fractures of the shaft and base of the 2ndmetatarsal are reasonably common overuse bone-related injuries in the athlete. However, fractures at the head of 2ndmetatarsal are rare. The first part of this series describes the case history of an elite level football player who has some well defined risk factors for a stress fracture of the 2ndmetatarsal. Part two of this series will focus on management of stress fractures of the 2ndmetatarsal as seen in this case study.
References
- J Orthop Sci 2003;8:273–8
- J Sports Med 1975;3:212–17
- Clin Sports Med 1985;4:737–52
- J Bone Joint Surg [Br] 1985;67:732–5
- Clin Sports Med 2006;25:139–50
- Clin Sports Med 1997;16:319–38
- Br J Sports Med 2016;50:471–475
- J Bone Joint Surg Am, 1985. 67:1372–1375
- Foot Ankle Int 1996;17:89–94
- Phys Med Rehabil Clin N Am 2006;17:813–26
- Int JSports Med, 2006. 27(6):493– 499
- Clin Orthop 1977;122:18–27
- Am J Sports Med 1989;17:669–74
- Foot Ankle Int. 2009;30:998-1004
- Bone 2005;37:253–60
- Am J Sports Med 2004;32:1893–8
- Med Sci Sports Exerc. 1999;31(Suppl 7):S448–S458
- J Am Acad Orthop Surg 2000;8:344–53
- Brodsky JW, Krause JO. Stress fractures of the foot and ankle. In: DeLee JC, Drez D, Miller MD, eds. DeLee and Drez Orthopaedic sports medicine:principles and practice.2nd edn. Philadelphia: Saunders, 2003;2:2391–408
- Am J Sports Med 2001;29:100–11
- Br J Sports Med 2007;41:510–514
- Journal of Athletic Training 2002;37(3):306–314
- Semin Roentgenol. 1994;29:176–193
- AJR Am J Roentgenol. 1992;159:245–252
- Am J Sports Med. 1987;15:46–58
- Am J Sports Med 1980;8:123–5
- Currey J. The Mechanical Adaptations of Bones. Princeton, NJ: Princeton University Press; 1984
- Am J Sports Med. 1984;12: 488–491
- Med Hypotheses. 1999;53:363–368
- 1977;269:80–82
- Calcif Tissue Int. 1993;53(suppl 1):75–81
- Calcif Tissue Int. 1984;36(suppl 1):56–61
- Int Orthop 2010;34:51–5
- Am J Sports Med. 1996;24:118–122
- Am J Sports Med 2004;32:1535–7
Newsletter Sign Up
Subscriber Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Be at the leading edge of sports injury management
Our international team of qualified experts (see above) spend hours poring over scores of technical journals and medical papers that even the most interested professionals don't have time to read.
For 17 years, we've helped hard-working physiotherapists and sports professionals like you, overwhelmed by the vast amount of new research, bring science to their treatment. Sports Injury Bulletin is the ideal resource for practitioners too busy to cull through all the monthly journals to find meaningful and applicable studies.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Injury Bulletin brings together a worldwide panel of experts – including physiotherapists, doctors, researchers and sports scientists. Together we deliver everything you need to help your clients avoid – or recover as quickly as possible from – injuries.
We strip away the scientific jargon and deliver you easy-to-follow training exercises, nutrition tips, psychological strategies and recovery programmes and exercises in plain English.







